Category Archives: Uncategorized
A Mother’s Story: When Your Child is Diagnosed with an MPN
 No one can prepare you for a cancer diagnosis of a child. Our daughter was four years old and began to complain about headaches. I assumed it was her eyes and made an appointment with an optometrist. Her sight was perfectly normal. A visit to her pediatrician lasted an hour with little insight, only suggestions to watch her diet, limit TV time and give her lots of water. She rarely watched TV and carried water with her throughout the day. Our diet doesn’t include sugar except from fresh fruit and we don’t eat boxed or canned food. I wasn’t optimistic. Eventually, her headaches became more severe on occasion, similar to migraines. We were sent to a neurologist. He requested blood work after she underwent an MRI. Thankfully, the blood work identified the problem-ET or essential thrombocythemia. We had never heard of it and had no idea what this meant for the future. A hematologist became our savior. With the proper diagnosis and medication, our daughter began to feel better, albeit a few side effects from the meds. Yogurt is a staple to help with GI issues, and a nap and early bedtime help fatigue. Yes, our little girl had what I would call fatigue. Our lives have changed but we do not let her ET control us. We control her ET. We manage her diagnosis as part of our daily lives as we would manage any other chronic disease. That is not to say it’s been easy. We have our moments of fear and doubt, but that doesn’t last as long as it used to. We keep very good records of her doctor visits, her blood levels and her overall health. We ask how she is feeling and pay attention to any changes that could be due to her ET. She is now 12 and enjoying a normal childhood. We are looking at Interferfon as a possible “next protocol,” if we think it will be better for her. We stay informed and are very pleased to see all of the clinical trials and new drugs on the horizon. It’s easy to say don’t panic if your child is diagnosed with an MPN. I would simply say, gather the facts, stay informed, be the voice they cannot be, and remember to take good care of yourself.
No one can prepare you for a cancer diagnosis of a child. Our daughter was four years old and began to complain about headaches. I assumed it was her eyes and made an appointment with an optometrist. Her sight was perfectly normal. A visit to her pediatrician lasted an hour with little insight, only suggestions to watch her diet, limit TV time and give her lots of water. She rarely watched TV and carried water with her throughout the day. Our diet doesn’t include sugar except from fresh fruit and we don’t eat boxed or canned food. I wasn’t optimistic. Eventually, her headaches became more severe on occasion, similar to migraines. We were sent to a neurologist. He requested blood work after she underwent an MRI. Thankfully, the blood work identified the problem-ET or essential thrombocythemia. We had never heard of it and had no idea what this meant for the future. A hematologist became our savior. With the proper diagnosis and medication, our daughter began to feel better, albeit a few side effects from the meds. Yogurt is a staple to help with GI issues, and a nap and early bedtime help fatigue. Yes, our little girl had what I would call fatigue. Our lives have changed but we do not let her ET control us. We control her ET. We manage her diagnosis as part of our daily lives as we would manage any other chronic disease. That is not to say it’s been easy. We have our moments of fear and doubt, but that doesn’t last as long as it used to. We keep very good records of her doctor visits, her blood levels and her overall health. We ask how she is feeling and pay attention to any changes that could be due to her ET. She is now 12 and enjoying a normal childhood. We are looking at Interferfon as a possible “next protocol,” if we think it will be better for her. We stay informed and are very pleased to see all of the clinical trials and new drugs on the horizon. It’s easy to say don’t panic if your child is diagnosed with an MPN. I would simply say, gather the facts, stay informed, be the voice they cannot be, and remember to take good care of yourself.
Click here to learn more about Pediatric and Young Adult MPNs
A Patient’s Story: What Box Do I Fit In And Does It Even Matter?

Linda, Grandmother and MPN Patient pictured above with her granddaughter.
I’m 58 and the proud mother of five beautiful children, their families and seven grandchildren. In 2017, I was diagnosed with essential thrombocythemia (ET). Looking back, I believe my symptoms began in 2011. I worked in a college library where I did research and helped organize lectures on various subjects for students and faculty. I also taught voice at night at a music school and sang at charity events and with various bands. Life was good. One day I got up from my desk and went to help students in the computer lab when all of a sudden everyone was a complete blur. Later, I experienced similar problems when teaching breathing techniques at the music school. I was in perimenopause so I wrote it off.
On Mother’s Day in 2011, I was out enjoying a band at a restaurant and while they were setting up their speakers, one blew right by my ear. I felt like I was underwater for an hour. Later that week I got a cold and had a loud heartbeat sound (pulsatile tinnitus) in my left ear. I then began a journey of symptoms that have not changed to this day. Early on I was diagnosed with various possibilities, Meniere’s Disease, MS, Vestibular Neuritis, Vestibular Migraine, maybe Lyme- so many ideas were entertained. I tried working for years in a reclined chair at my job. If I got up quickly without thinking, I would often see black spots. I would get odd brain fog at times and blamed it on the various drugs I was taking. After getting bounced around from neurologists to ENTs to cardiologists, I was finally diagnosed with atypical Vestibular Migraine.
In 2017, my platelets started climbing and my local neurologist, who had spent hours with me testing my blood pressure in different positions, felt I had a form of dysautonomia called POTs and needed more testing. He repeated an electromyography (EMG) study which showed severe neuropathy in 2012 and it came back the same in 2018. Eventually, I got to the point that the feeling of fainting was so strong I couldn’t stand. I tried to hide it whenever I could because it was so inexplicable even to myself. I was anxious because I never knew when a symptom would occur when I had to be up for any length of time and I looked normal on the outside and was embarrassed. My family and friends were frustrated with me because I went from being an active mom and grandmother to being disabled and limited in what I could do. My local neurologist sent me to a hematologist who diagnosed me with ET, CALR 1 mutation. He told me I would need a biopsy to confirm which I did at Sloan Kettering.,
As scary as it is to get diagnosed with a rare blood cancer, I felt slightly relieved that it might explain some of my symptoms and was told there was hope on the horizon with these blood cancers. It seemed that my neurological symptoms could not all be explained by the MPN only. and I probably have something else going on. I noticed that is a common complexity of MPN patients, we usually have other things going on and have been to many types of specialists. Being treated as a whole person can be challenging for us. I noticed that a lot of the symptoms were shared by the other groups I belonged to especially the Vestibular Migraine Group and Pots. It occurred to me that if these different chronic illnesses could be studied together maybe drugs used to help one could be used to help another especially if you are in a “watch and wait” situation. I’m sure this is being done all over the world.
I realized after joining some of the social media groups, that I am not alone in this feeling especially when it comes to the atypical migraines, brain fog and dizziness. Being in a box, is not so important anymore. Especially in the MPN world where you can have one type one day and potentially can learn it progressed or changed to another. We are in this together. No matter what. I’ve been lucky to have been referred to the Cleveland Clinic where I’m being evaluated by neurology and oncology to come up with an answer. I’m inspired by that institution and the kindness of everyone from the shuttle drivers, to the technicians and doctors who work there.
If I had any advice to share it would be to be your own advocate. Not believing everything you read in the groups is also important because it may never be part of your story and there is so much being researched and studied. If anything happens to be written that is inaccurate, you can put yourself in a state of fear even if you try to tell yourself otherwise. Also, there are wonderful friendships to be made with people who know what you are going through. I’m looking forward to finally meeting a fellow MPN patient, who I have been communicating with for a year at MPN Advocacy & Education International’s program in Cleveland this November. I’m realizing the importance of yoga and nutrition and I still try to keep busy for as long as I can stand before I give myself permission to rest when I can’t. I’ve since learned that life is unpredictable and can change in a moment. All in all, I try to be optimistic and feel most people are kind, loving, and caring, but no one knows what you feel better than yourself. I’ve also learned I have the best family, friends, and people in my life who provide love and support.
Health Insurance: What You Should Know
By Pam Trexel, American Cancer Society, Senior Vice President, Alliance Development and Philanthropy

Pam Trexel
Access to health care is a significant determinant in whether an individual diagnosed with cancer will survive. Uninsured individuals are more likely to be diagnosed with cancer at a later stage and more likely to die from the disease. The American Cancer Society Cancer Action Network (ACS CAN), the public policy arm of the American Cancer Society, believes all Americans should have access to affordable, quality health insurance.
Fortunately, in recent years there has been an increase in the number of Americans who have health insurance coverage. Since 2014, Americans have had access to comprehensive coverage that includes key consumer protections vitally important to cancer patients. These protections include: prohibiting insurance companies from denying coverage or charging more due to a consumer’s pre-existing conditions, restrictions against insurers imposing arbitrary caps on coverage, and a requirement that all insurance offered to individuals cover a broad set of benefits called essential health benefits.
Yet there are still challenges. Many cancer patients have difficulty finding specialists who participate in their insurance plan’s network, affording their prescription medications, and understanding their out-of-pocket expense liability. Recent regulatory and legislative approaches on both the federal and state levels have the potential to weaken current patient protections, segment the insurance market, allow for more insurance plans with inadequate coverage, and reduce access to healthcare for cancer patients and survivors.
Federal Activities
In 2018 the administration finalized a rule that would expand access to short-term, limited-duration (STLD) policies. The rule allows STLD products to be sold for a coverage period of up to 12 months and be renewed for three years. ACS CAN urged the administration to withdraw the rule due to concern that these policies are exempt from many of the key patient protections that ensure individuals with cancer and survivors have access to quality health care needed to treat their disease.
Additionally, the current administration has repeatedly reduced enrollment education and outreach funding,which limits efforts to inform consumers about open enrollment and plan options. Concerns remain about enrollment trends in future years and the abilities of non-governmental groups to continue outreach and enrollment efforts.
State Activities
Faced with uncertainty from the federal government, some states have implemented policies that seek to either strengthen or weaken the individual health insurance market.
Short-Term Limited-Duration Policies
As federal regulations try to expand access to STLD policies, some states are trying to prohibit or minimize their expansion. For example, New York state law permits the sale of short-term limited duration policies, but requires these plans abide by the consumer protections required for ACA-compliant plans.Other states are considering legislation that would limit STLD policies to a coverage period of less than three months without the option for renewal.
State Individual Mandates
The federal individual health insurance mandate penalty ended January 1, 2019. In response a few states have begun considering state-level individual mandates requiring state residents to maintain health insurance. Massachusetts has had a state individual insurance mandate since before the implementation of the ACA and never rescinded it. New Jersey has also enacted legislation to impose an individual mandate requirement.
Non-Comprehensive Coverage
Following administrative actions encouraging creation of association health plans (AHPs) – plans wherein small businesses join together to purchase health coverage – some states are considering legislation that exempts AHPs from state regulation. These plans are already exempt from the important patient protections provided under the Affordable Care Act (ACA). ACS CAN is concerned these plans will be able to discriminate against people based on their health status and will syphon off younger, healthier people, leaving older and sicker people in the state’s individual market (which would increase premiums).
Utilization Management
Cancer patients often need to choose a health plan based, in part, on the plan’s prescription drug coverage. Utilization management programs are health insurer practices used to control spending. These practices may include: prior authorization or approval of a drug by the patient’s health insurer before a prescription can be filled; and step therapy which requires patients to try, and fail, on an insurer-chosen prescription drug before gaining access to the drug that was prescribed by their doctor but may be more expensive. ACS CAN is concerned that if used inappropriately, utilization management may delay care or impede access to prescription drugs for cancer patients. Several states are considering legislation to ensure that utilization management practices are timely, efficient, clearly described for both patients and doctors, and allow for appeals and exceptions when appropriate.
Special Interview: Living with an MPN in Childhood
Diagnosed at age seven with Essential Thrombocythemia, Portia shared her story at the 2nd Annual Pediatric & Young Adult MPN Patient Program.

Portia, a young adult MPN patient, shared her story at the 2nd annual Pediatric & Young Adult Program
Do you remember experiencing any symptoms?
I had occasional nosebleeds that would last about twenty minutes or so. But over time, the time decreased to about ten minutes. I also experience fatigue, especially when I’m sick, all I do is sleep to try and regain any energy. Also, I’m very active and I play competitive squash, so I do experience fatigue more than an average person.
How do you cope with essential thrombocythemia (ET) symptoms and/or side effects from Hydroxyurea?
I’m very lucky that I don’t really experience too many symptoms, but I usually push through any pain that I have since I’m such a wimp about medication. I have not had any side effects from Hydroxyurea. For fatigue, I don’t take any other medication, I pretty much just work hard and try to be smart about how I utilize my energy. When playing squash, I work extra hard to make up for my fatigue, but if I really can’t breathe due to lack of oxygen, I will talk to my coach and ask for a small break to recuperate. Most coaches are very reasonable and will allow a break.
Has ET curtailed your involvement in school activities? Sports?
When I was younger, elementary and middle school age, I would occasionally have to miss school for lab appointments, so I would have to make up work. One symptom of ET is fatigue, so I do have to deal with that in sports. But I also have Hemoglobin H, which I believe has a bigger impact on my fatigue in sports than ET. But overall, I still go about my life and continue to do the things I love.
How do you explain what you have to your friends?
As I’ve gotten older, I’ve done a lot more of my own research to further understand my condition, but to my friends, I explain that I have way too many platelets, which help clot your blood when you get a cut, and because of that, I bleed for longer.
What advice would you give other younger individuals with an MPN when peers say they don’t look sick or they’re faking?
I would tell them to do their best to ignore their hateful comments and try to explain their condition by telling them it’s something internal rather than external, that’s why they don’t appear sick. And most important, find friends who won’t judge you, and people who do, clearly aren’t your real friends, for real friends should accept you no matter what.
You are very energetic and positive, when you reach out to others your age who aren’t feeling well, what do you say to encourage them?
First, I would listen to their concerns and possible issues, and then I would tell them to keep their head held high and know that it does get better. This is just a phase and eventually, the negative parts will fade away. Also, it’s very important to know who your close friends are and be able to talk to them since many kids would rather talk to their friends rather than a parent or even a doctor since it can be intimidating. I would also say, take one day at a time and find joy in the little things, whether it’s going for ice cream or just taking a nice walk.
If you could wave a wand and change one thing in the world of MPNs, what would you change?
Personally, I would change the medicine. I really hate swallowing pills, so I would much prefer something fun to eat or drink as my medicine. I’m also very strange and would much rather have the medicine get injected into me, which I know is an option, but the majority of people aren’t a big fan of needles.
A Caregiver’s Story: The Journey of a Spouse Through the Transplant Process
In March, MPN Advocacy & Education International highlighted the story of a recent stem cell patient, Andrea (click here to view story). This month, Andrea’s wife, Denise, shares her story as a caregiver in an interview with us.

Andrea and Denise
How did you feel about your spouse’s decision to have a transplant? Were you apprehensive?
I have been a part of Andrea’s medical journey since her diagnosis from ET to myleofibrosis. I recall it took me about a week to learn how to pronounce the name correctly, and it has been an education ever since. Being present during doctor appointments and multiple clinical trials provided first-hand information in addition to our ongoing discussions. Observing and experiencing her five years of transfusion independence was a gift. We took advantage of the opportunity to cycle and travel together and separately. Knowing the clinical trial would either end or the drug would quit working was only a matter of time. And knowing how she physically felt prior to and after this time period played a role in my ‘wrapping my head’ around a possible future transplant. All the while, we adjusted and modified activities as needed in order to continue allowing her to live life to the fullest.
When medications were no longer yielding the same results, and Andrea’s blood transfusions became more frequent, the doctors felt the alternatives were to continue clinical trials and hope for the best or discuss a stem cell or bone marrow transplant. I felt she was strong enough physically to beat the odds. It was now or never. I never doubted our decision, and have had no regrets.
How did you prepare yourself as a caregiver?
In order to prepare, I scoured MD Anderson’s educational resources to understand what a ‘typical’ transplant journey would entail. I developed multiple spreadsheets to track medications, nutrition, recovery, therapy, etc. I left the online myleofibrosis forum readings to Andrea as she would report her findings from reading first-hand accounts. She also talked to many individuals who had had transplants, pummeling them with questions.
Another important piece of this journey was my mindset. I focused on the end goal – her successful transplant and healthy recovery. I looked at the journey in three parts:
- Pre-transplant
- Transplant/hospital stay
- Post-transplant
My goal was to have as much of her daily care and needs become second nature to me prior to her hospital release. When she was released, the additional environmental interaction was familiar without the distraction of ‘everything new all at one time’.
What tools did you find useful as the caregiver and advocate?
I created a 3-ring notebook with tabs to manage spreadsheets, medical records/test, and doctor questions, so I could access information easily and quickly. I created a spreadsheet to track her medication schedule. The purpose was to help me identify what was needed, including dosage when refilling medications both inside and outside the hospital. Click here to view medication tracker template. (For an Excel spreadsheet version of the attached please email kmichael@mpnadvocacy.com).
I also knew there was a good possibility that after her hospital release and within the first 100 days, she would have a trip to the emergency room and be re-admitted to the hospital. Therefore, medications and ‘the notebook’ were kept in one location and easily picked up and transported with us. The notebook was with us each time we visited the care team.
I created additional spreadsheets to help track:
- Food and water daily intake and output. This is useful for doctor & nutrition appointments.
- Daily stats: blood pressure, temperature, pain levels, exercise, spirometer therapy. This is useful for tracking blood pressure and temperature anomalies. Because if her temperature rose to a specific number, she had to go to the emergency room immediately.
- Signs of graft vs host disease (GVHD).
- I choose to stay in the hospital 24/7 to understand how the nursing staff/care team handled her care. This experience helped me understand her routine.
- I figured if I learned her hospital routine, it would be familiar when she was released.
- I used my smartphone and set alarms with labels so I knew what drugs were due when. (Used upon hospital release.)
- I utilized Caring Bridge (www.caringbridge.org) to communicate Andrea’s transplant journey to her friends and family. My intent with each post was to create an engaging story yet convey “a day in her life” so everyone could get a sense of being there.
What was the most challenging part of your role and why?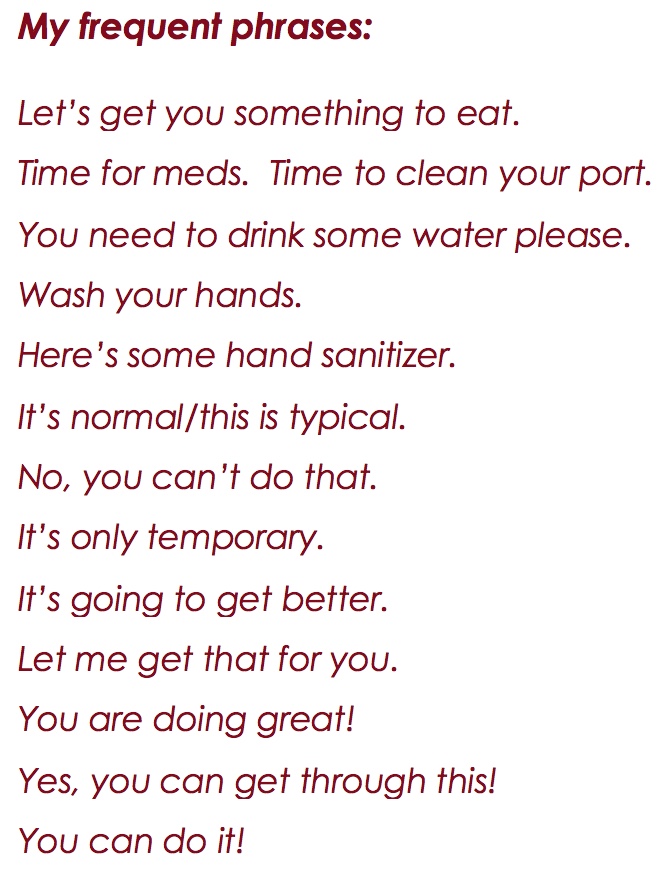
Coming home and changing environments automatically kicked us back to normal behaviors and patterns. I felt we had to be more careful and diligent in preventing infection. Even though we were home, I had to be more watchful because familiarity brings about a relaxed state. Her immune system was developing and the risk of infection was too great. Andrea quickly tired of me saying “No, you can’t do that or touch that.”
Once home, Andrea’s friends visited. This was a considerable risk to her because the natural tendency is to hug and touch. To reduce her risk, we asked people to use hand sanitizer when they were around her. We developed a routine where I would greet her friends first with a hug and explain she couldn’t hug yet. Andrea stood back a few feet to reduce her availability.
What I learned :
Every recovery and journey is different.
While it’s tempting, don’t measure your progress against someone else. It’s your journey. That goes for both the patient and caregiver!
The “notebook” was a great tool. It kept us on schedule for all medications and were able to provide information to the doctors as needed.
The hospital care team staff is a critical part of your recovery. Don’t opt for staying close to home if you feel a facility’s care team is better in another location.
Deciding where to have the transplant included researching the number of myleofibrosis transplants, versus other blood disease transplants, and the success that facility had.
Participate in the journey. I chose to shave my head at the same time Andrea did. It sure made showering quick and easy!
Take in the outdoors and/or change the scenery.
Exercise or go for walks. Listen to music. Visit a friend. Go to the grocery store. Do something to clear your head and regain perspective.
Have a confidante. It’s normal to question, or become frustrated, and to second guess. But remember – it’s temporary.
You are the coach, cheerleader, and guardian all at once. Embrace the many hats you will wear!
Click here to read Andrea’s Transplant Story
MPN Patient Daily Stats 06-10-18
A Veteran’s Story Told By His Wife

Bill C. Veteran and MPN Patient
In January 2017, my husband, Bill, was enjoying his consulting business and writing a book that has been in his mind for years, when an annual physical changed everything. Some lab work was “off” according to the Veterans Administration (VA) physician so Bill sent the lab results to our personal physician, who is also our best friend. Within ten minutes after receiving it, our friend asked Bill to come to his clinic immediately. Further blood tests yielded an initial diagnosis of Chronic Myeloid Leukemia (CML).
While we were reeling from that shock and trying to ground ourselves, our physician friend sent us to a local hematologist for additional work-ups and treatment. Following a bone marrow test, we were further shocked to find out that the CML we had become somewhat resolved with was indeed Myelofibrosis (MF). We sat in a dumb stupor trying to figure out what that was, how serious it was, where it came from, what we could do about it, etc. We were encouraged to start on the only medication for Myelofibrosis, Jakafi, and were told the only drawback to the drug was its cost–$10,000/month! We immediately started working with the VA for them to supply the medication. After numerous telephone calls and in-person visits with both our hematologist and the VA (in a city 40 miles from our home), we secured VA support for Bill’s Jakafi. It now routinely comes to our home in an innocuous package. The initial symptoms Bill was experiencing responded to the Jakafi but so did the platelets and hemoglobin which are continuing to drop so we played with the dosage to, hopefully, continue to drive the white blood count down while keeping the platelet count and hemoglobin up closer to where they should be. The drop in Jakafi was too drastic and symptoms immediately returned so our local hematologist moved Bill back to the original dosage. Symptoms once again are gone and platelets somewhat controlled but still very low. Hemoglobin is recovering which is good.
 While all of this was going on, we decided, with the support of our local hematologist (who is wonderful realizing this is all about Bill and not about the hematologist’s ego), to go to Rochester, MN to Mayo Clinic to see one of the leading researchers in Myelofibrosis, Dr. Tefferi. While there was no proactive guidance offered from this visit, we did learn that we should only approach researchers whose field of study is a fit between their interests and Bill’s current health status. To that end, we went to Northwestern University in Chicago to see Dr. Brady Stein, another renowned Myelofibrosis researcher. He listened and answered all of our questions while assessing Bill’s fitness for ongoing clinical trials. His ultimate recommendation was for us to consider a transplant—again, another shock as we had hoped that we would have a variety of alternative treatments Dr. Stein is concerned that Bill’s Next Gen Sequence report that showed other mutations limit the time he will have before he converts to Acute Myeloid Leukemia (AML). Since Bill is in such good health right now (ironically), Dr. Stein found him to be amongst 10% of people with MF that even qualify for a transplant consultation and while a transplant is a “rough ride” encouraged us to explore it.
While all of this was going on, we decided, with the support of our local hematologist (who is wonderful realizing this is all about Bill and not about the hematologist’s ego), to go to Rochester, MN to Mayo Clinic to see one of the leading researchers in Myelofibrosis, Dr. Tefferi. While there was no proactive guidance offered from this visit, we did learn that we should only approach researchers whose field of study is a fit between their interests and Bill’s current health status. To that end, we went to Northwestern University in Chicago to see Dr. Brady Stein, another renowned Myelofibrosis researcher. He listened and answered all of our questions while assessing Bill’s fitness for ongoing clinical trials. His ultimate recommendation was for us to consider a transplant—again, another shock as we had hoped that we would have a variety of alternative treatments Dr. Stein is concerned that Bill’s Next Gen Sequence report that showed other mutations limit the time he will have before he converts to Acute Myeloid Leukemia (AML). Since Bill is in such good health right now (ironically), Dr. Stein found him to be amongst 10% of people with MF that even qualify for a transplant consultation and while a transplant is a “rough ride” encouraged us to explore it.
To that end, we have met with Dr. Tom Chauncey who is the Program Director at the VA in Puget Sound-who along with the University of Washington at Seattle are the number one transplant center (particularly for people with MF) in the country. Dr. Chauncey was very generous with his time and counsel and offered to work with us as we continue to explore transplant options. With Dr. Stein’s support, we also will meet with the Director of the Northwestern University Transplant Program, Dr. Mehta.
Simultaneously, we filed a VA benefits claim related to Myelofibrosis, believing Bill’s exposure to Agent Orange most likely caused this illness, but we were denied. Bill is a Vietnam Veteran having served in Quang Tri—I Corp from November, 1968 – November, 1969 and was exposed to Agent Orange/Dioxin. While compiling our appeal information, we found numerous Citations where the VA had granted benefits for veterans (on appeal) who have been diagnosed with Myelofibrosis due to exposure to Agent Orange, so will be using that information to move our claim forward. During the exploration for more information, we also discovered that the VA is finalizing a rule to add to the benefits structure Stem Cell Transplant coverage as well as treatment protocol to include myelosuppressive therapies of which Jakafi is one. This proposed change is set to take effect in FY18 (which begins as soon as October 1, 2017) which is exciting for veterans waiting for coverage of Myelofibrosis because, at least, some of the symptoms and associated therapies will be addressed.
MPN Advocacy & Education International continues to advocate for essential thrombocythemia, myelofibrosis and polycythemia vera to be included in the VA’s ‘presumptive’ list of illnesses related to Agent Orange exposure. Please click here if you are in the process of filing a claim or appealing a claim for more details.
Like many of you, we are sure, our world right now is exploring drugs in Phase II or III of clinical trials that are successful in producing remission in MF as well as other drug trials/existing drugs that will hold down the “blasts” that would otherwise convert Bill to AML. We are also exploring transplant centers, protocol, outcomes, experiences, etc. to get a better sense of whether that is something we even want to consider.
In the midst of all of this, we continue to work hard to enjoy our lives. Having a daughter with Down Syndrome who is now 43 years old taught us that nothing is ever guaranteed and that we would have to fight for anything and everything we wanted. We “cut our teeth” on the fights for our daughter, Mindie, against insurmountable odds and won. Now we are using those skills on Bill’s behalf. While sad and scared, we remain determined that there are many, many opportunities for Bill to remain as healthy as he is today and live a long and enjoyable life beyond the current prognosis. We know there is a lot to learn from all of you “in our same boat” and look forward to sharing stories and guidance between all of us. In the interim, all of you touched by an MPN are in our thoughts and prayers. Together we can change the face of these diseases!
A Patient Story: Living 32 Years with an MPN
By Ron K.
 Fortunately, my MPN journey has been a long one. I was first diagnosed 32 years ago and I know have post-Polycythemia Vera Myelofibrosis. Looking back it was almost archaic in nature. Today the progress has been immense on many fronts, not just in treatment, but with treating the patient as a whole. As many of you know, there is no exact recipe book for life with cancer and its treatment journey is unique. My hope is that sharing some of my experiences may help someone else along the way.
Fortunately, my MPN journey has been a long one. I was first diagnosed 32 years ago and I know have post-Polycythemia Vera Myelofibrosis. Looking back it was almost archaic in nature. Today the progress has been immense on many fronts, not just in treatment, but with treating the patient as a whole. As many of you know, there is no exact recipe book for life with cancer and its treatment journey is unique. My hope is that sharing some of my experiences may help someone else along the way.
There is a quote by Albert Einstein that reflects my approach to my medical journey
Learn from yesterday, Live for today, Hope for tomorrow. The important part is to not stop questioning.
Learn, Live, Hope – three good words for any cancer patient.
As those with an MPN know this is a chronic neoplasm and unfortunately there is no treatment yet to cure this illness. Some of the latest MPN and MF drugs do improve one’s quality of life and even appear to extend one’s survival, a significant milestone from what was available just a handful of years ago. Finding ways to slow or stop the progression is my only hope until medical knowledge can surpass me with a real solution.
Having a chronic cancer and having it for a long time has enabled and encouraged me to evolve into a healthier lifestyle. One does not have to change everything overnight but just evolve and continue to build healthier ways, one step at a time. While there is no evidence that a healthy lifestyle will cure me, it is something I can do and have control over.
This all started back in 1985 when I went to my family doctor with a cold and I mentioned that my colds seem to last longer and hit me harder than others. A simple blood test began my journey. I would not be alive today if I followed my first hematologist’s treatment plan. He wanted to treat me in a traditional manner at that time, with a radio isotope that kills off some of the marrow, they know now that treatment leads to an acute leukemia years down the road. Instead my intuition questioned this approach, since I was only 31 and I thought that I might need that marrow later in life. I called a major metro medical center and asked for an appointment with their Chief of Hematology. Unknown to me at the time, and not commonly termed in the 1980’s, I was going to get something called a second opinion. I got an appointment and his approach was quite different. He wanted to understand me, my rate of progression, severity, etc as that would lead him to figure out how to best treat me. He even commented that the current radio isotope treatment (my first hematologist’s plan) to kill off marrow was likely going away as he saw it.
Today, I am a patient of Dr. Mesa’s. I found that they could answer all my questions. Answers to questions that my previous hematologists could not answer. They have knowledge that is very leading edge as to direction of MPN treatments as they are part of an elite group of hematologists that are making many of the MPN discoveries, designing the clinical trials and studies with other key hematologists around the world. So my personal doctor advice is to make sure you find the right doctor and treatment strategy for you. Listen to your intuition and ask questions, seek information and acquire knowledge in your cancer and health. Expect answers or find those professionals that can give them to you. While I did not need a MPN specific doctor early on I do need one now as I am living well beyond the averages.
For me, finding the right doctor has been a key in my cancer treatment journey. Getting a second opinion is also key. What you will likely find is the different doctors will agree on the diagnosis but their treatment strategy will often be different.
I attend conferences, seminars, and special programs such as those that the MPN Advocacy and Education International puts on. I have done online webinars or conferences as well as belong to online MPN listing groups to learn and share information. I find this information to be helpful to ask the right questions to my doctors and understand what may be option in the future.
I believe support makes a difference. It is helpful to have support from your spouse, kids, parents or friends. I also find that support groups can be very helpful as well. As they can fill a support void that is missing from one’s non-cancer family and friends. This is no fault of family, spouses, or friends in that they do listen and they do try to understand and relate and they do support the cancer patient, but I have found that belonging to a cancer support group often helps to fulfill things non-cancer patients cannot quite grasp. I have belonged to both hematology specific support groups and all cancers support groups. You might want to try both and see if one works better than another.
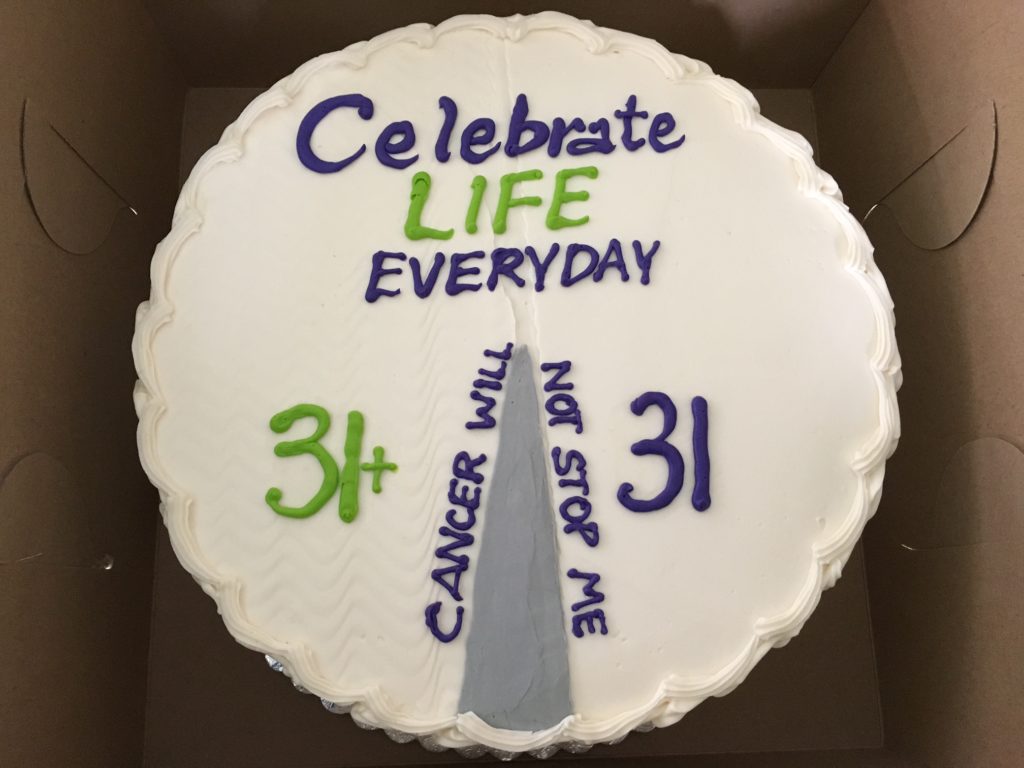
As I live my life, I am grateful for every day. Everyday is a great day, just some are even better than others. I even celebrated the point in my life where I have lived longer with cancer as part of my life than without cancer. That was at about 31 1/2 years and I had a bakery make me a cake to celebrate the occasion. The cake was symbolic of my MPN journey and view of life. I celebrated this occasion with my all cancer support group. So while cancer is a part of my life I run my life with cancer being a part of it and I do not let my cancer rule over me. I am hopeful that a cure is in our much sunnier MPN journey. May the best be yet to come, and enjoy the day!
Tips for Caregivers
Suggestions for being an effective caregiver
Caring for a person with cancer may seem complex and like too much to cope with at first. Depending on the person’s needs, you may provide different types of support, such as:
- Emotional support
- Help with medical care
- Assist with financial and insurance issues
- Serve as the communicator between the patient and the health care team
You may find the following tips can help you become a successful caregiver:
Remember that caregiving is a team effort. A caregiver is a member of an important team of family members, friends, volunteers, and the health care team. Each member of the team offers different skills and strengths to provide effective care.
If you are the main caregiver, help each team member express concerns, opinions, and emotions. Also, make sure that the person with cancer has a central role in all discussions and decisions, if possible. It is very important for the person with cancer to feel like an active member in their care.
CancerCare provides a special website for caregivers called My Cancer Circle. This website can help caregivers organize the family and friends who want to help. Find other online communities for support.
Create a list of tasks. Caregiving, like any responsibility, involves tasks of varying importance. Start by making a list of all of your caregiving tasks. Then, use it to decide how to divide the tasks between friends, family, professionals, and other volunteers.
Be proactive. Being proactive means taking charge and planning as much as possible to prevent last-minute emergencies. This can also help provide a sense of control and order. Create schedules that list which relative, friend, or other volunteer is available when and for what tasks. Make sure that all of the caregivers involved have some time to be away without feeling guilty or concerned. Long-distance caregiving takes even more planning. Find out more about how to be an effective long-distance caregiver.
A Patient’s Story: My Clinical Trial Experiences
At what point in your MPN diagnosis did you join a clinical trial? What trial (drug) were you in?
I was diagnosed with PV in 2001. Only on phlebotomy and 81mg aspirin until 2007 when I began hydroxyurea because I turned 60 in 2006 and was now “high risk.” In 2009 my spleen was enlarging. I had been hearing that Interferon was best taken in the early stage of MF and might reduce myelofibrosis. My hematologist advised me he would be having a trial with Pegasys (Interferon) and I should wait for that. I actually waited until 2012 when the trial became available. I was now showing signs through bone marrow biopsies of secondary MF.
Did you feel as though you received accurate information getting into the trial?
Yes, I had been reading about Interferon treatment and knew I wanted to try it. Perhaps I didn’t know how quickly I could be removed from the trial because of my worsening symptoms.
What didn’t you know going into the trial that would be useful for others to know or questions they might ask?
It would have helped to know at what point you may be pulled from the trial and what happens after you are removed. Also, I did not know that the FDA can shut a trial down at any point due to adverse reactions to few patients.
How many clinical trials have you participated in?
I am currently on my 3rd clinical trial. (First trial wasn’t improving my symptoms, second trial was shut down by the FDA and the pharma company decided not to proceed , and the third trial I have begun my 4th year.)
Were you able to get the drugs after the trial(s) if you were doing well?
I can continue with the drug I am currently on as long as I continue to have benefit and as long as there is funding for this drug by the pharma company, and that it doesn’t get shut down prior to FDA approval
What advice would you impart to those who are skeptical about clinical trials who are not doing well on available treatments?
What do you have to lose? If you are currently not well, you certainly may have good results and feel better. If you don’t show benefit you will be removed to try something else. We do not know the future after taking these drugs. That is a gamble we must take.
Would you participate in other trials knowing what you know now?
If I was not feeling well and I met the qualifications, I would try again.
Marylin C. has been living with her diagnosis for many years. She has graciously volunteered for trials not only for her own reasons, but for the sake of MPN patients and their futures.
