Category Archives: Treatment
Interferons in the treatment of myeloproliferative neoplasms
Pankit Vachhani, John Mascarenhas , Prithviraj Bose , Gabriela Hobbs, Abdulraheem Yacoub, Jeanne M. Palmer , Aaron T. Gerds, Lucia Masarova, Andrew T. Kuykendall, Raajit K. Rampal, Ruben Mesa and Srdan Verstovsek
Abstract: Interferons are cytokines with immunomodulatory properties and disease-modifying effects that have been used to treat myeloproliferative neoplasms (MPNs) for more than 35 years. The initial use of interferons was limited due to difficulties with administration and a significant toxicity profile. Many of these shortcomings were addressed by covalently binding polyethylene glycol to the interferon structure, which increases the stability, prolongs activity, and reduces immunogenicity of the molecule. In the current therapeutic landscape, pegylated interferons are recommended for use in the treatment of polycythemia vera, essential thrombocythemia, and primary myelofibrosis. We review recent efficacy, molecular response, and safety data for the two available pegylated interferons, peginterferon alfa-2a (Pegasys) and ropeginterferon alfa-2b-njft (BESREMi). The practical management of interferonbased therapies is discussed, along with our opinions on whether to and how to switch from hydroxyurea to one of these therapies. Key topics and questions related to use of interferons, such as their safety and tolerability, the significance of variant allele frequency, advantages of early treatment, and what the future of interferon therapy may look like, will be examined. Pegylated interferons represent an important therapeutic option for patients with MPNs; however, more research is still required to further refine interferon therapy.
Navigating Cytoreduction in MPNs: Benefits, Risks, and Considerations
In an interview with Targeted Oncology, Douglas Tremblay, MD, discussed the significance of cytoreductive therapy in mitigating thrombotic risk in myeloproliferative neoplasms.
According to Douglas Tremblay, MD, cytoreductive therapy has emerged with a pivotal role in mitigating thrombotic risk in the treatment landscape of myeloproliferative neoplasms (MPNs), specifically essential thrombocytopenia (ET) and polycythemia vera (PV).
Despite the evident benefits, each therapy carries unique adverse effects, requiring the careful consideration of patient-specific factors in treatment administration. Deciding when to initiate cytoreductive therapy in patients with chronic MPNs relies on accurate risk assessment, with parameters such as age and prior thrombotic events often guiding treatment decisions.
Frontline therapies, such as hydroxyurea and interferon, manage blood counts for patients with ET and PV, and newer options are emerging, according to Tremblay, assistant professor of medicine at the Icahn School of Medicine at Mount Sinai. However, the long-term implications focus on thrombosis prevention and disease progression.
Ongoing research endeavors aim to delve deeper into surrogate end points and novel therapeutic avenues, promising to further refine and revolutionize the management of MPNs.
In an interview with Targeted OncologyTM, Tremblay discussed the significance of cytoreductive therapy in mitigating thrombotic risk in MPNs, specifically ET and PV.
Health Canada Slated to Review New Drug Submission for Momelotinib in Myelofibrosis
Health Canada has accepted for review the new drug submission seeking the approval of momelotinib in patients with myelofibrosis, according to a recent announcement from GlaxoSmithKline.1 The submission is based on findings from the phase 3 SIMPLIFY-1 (NCT01969838) and MOMENTUM (NCT04173494) trials.
Specifically, SIMPLIFY-1 data showed that of the 86 patients who received momelotinib, 31.4% (95% CI, 21.8%-42.3%) experienced a spleen volume response (SVR) reduction of 35% or higher vs 32.6% (95% CI, 23.4%-43.0%) of the 95 patients who received danazol.2
Moreover, findings from MOMENTUM indicated that a tumor symptom score (TSS) of at least 50% was observed in 25% of the 130 patients given momelotinib per the Myelofibrosis Symptom Assessment Form (MFSAF v4.0), representing a treatment difference of 16% (95% CI, 6%-26%; P < .01).2,3 The MFSAF v4.0 TSS change from baseline in the momelotinib and danazol arms were -9.4 and -3.1, respectively, equating to a difference of -6.2 (95% CI, -10 to -2.4; P = .001).
European Commission Approves Momelotinib for Myelofibrosis/Anemia
The European Commission granted marketing authorization to momelotinib (Omjjara) for patients with primary myelofibrosis who have disease-related splenomegaly or moderate to severe anemia, according to a press release from GSK.1
This indication also covers patients with post polycythemia vera myelofibrosis or post essential thrombocythemia myelofibrosis who are JAK inhibitor naïve or received previous treatment with ruxolitinib (Jakafi). The authorization is based on results from the phase 3 MOMENTUM trial (NCT04173494), which analyzed the use of momelotinib and danazol in patients with symptomatic and anemic myelofibrosis.2
“The challenges of living with myelofibrosis can be burdensome, and symptomatic patients can experience spleen enlargement, fatigue, night sweats, and bone pain. Until now, there have been no options specifically indicated to treat these symptoms in patients who also experience anemia. The authorization of [momelotinib] brings a new treatment option with a differentiated mechanism of action to these patients in the European Union,” Nina Mojas, senior vice president of Oncology Global Product Strategy at GSK, said in the press release.
In the trial, the total symptom score response at week 24 was 24.6% (95% CI, 17.49%-32.94%) for patients receiving momelotinib vs 9.2% (95% CI, 3.46%-19.02%) in the danazol arm (P = .0095). Additionally, a reduction of splenic volume by 25% occurred in 40.0% (95% CI, 31.51%-48.95%) of patients in the momelotinib arm vs 6.2% (95% CI, 1.70%-15.01%; P <.0001) in the danazol arm. A 35% reduction in spleen volume was also observed in 23.1% (95% CI, 16.14%-31.28%) in the momelotinib arm and 3.1% (95% CI, 0.37%-10.68%; P = .0006) in the danazol arm.
In September 2023, the FDA approved momelotinib for patients with intermediate- or high-risk myelofibrosis, including primary and secondary myelofibrosis, who are experiencing anemia.3 In November 2023, the European Medicine’s Agency’s Committee for Medicinal Products for Human Use expressed a positive opinion for momelotinib.4 The positive opinion was one of the final steps leading to the approval of the drug in the European Union.
“I think [momelotinib] will make an immediate impact. There clearly are individuals now who are on JAK inhibitors like ruxolitinib or fedratinib [Inrebic] who have significant anemia who will immediately be potential candidates,” Ruben A. Mesa, MD, FACP, said in an interview with CancerNetwork® prior to the FDA approval. Mesa is the president of the Enterprise Cancer Service Line and senior vice president at Atrium Health; executive director of the National Cancer Institute-designated Atrium Health Wake Forest Baptist Comprehensive Cancer Center; and vice dean for Cancer Programs at Wake Forest University School of Medicine.
References
- European Commission authorises GSK’s Omjjara (momelotinib). News release. GSK. January 29, 2024. Accessed January 29, 2024. https://shorturl.at/ntuvy
- Mesa RA, Gerds AT, Vannucchi A, et al. MPN-478 MOMENTUM: phase 3 randomized study of momelotinib (MMB) versus danazol (DAN) in symptomatic and anemic myelofibrosis (MF) patients previously treated with a JAK inhibitor. J Clin Oncol. 2022;40(suppl 16):7002. doi:10.1200/JCO.2022.40.16_suppl.7002
- Ojjaara (momelotinib) approved in the US as the first and only treatment indicated for myelofibrosis patients with anaemia, News release. GSK. September 15, 2023. Accessed January 29, 2024. https://shorturl.at/jnNQY
- GSK receives positive CHMP opinion recommending momelotinib for myelofibrosis patients with anaemia. News release. GSK. November 13, 2023. Accessed January 29, 2024. https://bit.ly/3MEYpOl
A Caregiver’s Story: The Journey of a Spouse Through the Transplant Process
In March, MPN Advocacy & Education International highlighted the story of a recent stem cell patient, Andrea (click here to view story). This month, Andrea’s wife, Denise, shares her story as a caregiver in an interview with us.

Andrea and Denise
How did you feel about your spouse’s decision to have a transplant? Were you apprehensive?
I have been a part of Andrea’s medical journey since her diagnosis from ET to myleofibrosis. I recall it took me about a week to learn how to pronounce the name correctly, and it has been an education ever since. Being present during doctor appointments and multiple clinical trials provided first-hand information in addition to our ongoing discussions. Observing and experiencing her five years of transfusion independence was a gift. We took advantage of the opportunity to cycle and travel together and separately. Knowing the clinical trial would either end or the drug would quit working was only a matter of time. And knowing how she physically felt prior to and after this time period played a role in my ‘wrapping my head’ around a possible future transplant. All the while, we adjusted and modified activities as needed in order to continue allowing her to live life to the fullest.
When medications were no longer yielding the same results, and Andrea’s blood transfusions became more frequent, the doctors felt the alternatives were to continue clinical trials and hope for the best or discuss a stem cell or bone marrow transplant. I felt she was strong enough physically to beat the odds. It was now or never. I never doubted our decision, and have had no regrets.
How did you prepare yourself as a caregiver?
In order to prepare, I scoured MD Anderson’s educational resources to understand what a ‘typical’ transplant journey would entail. I developed multiple spreadsheets to track medications, nutrition, recovery, therapy, etc. I left the online myleofibrosis forum readings to Andrea as she would report her findings from reading first-hand accounts. She also talked to many individuals who had had transplants, pummeling them with questions.
Another important piece of this journey was my mindset. I focused on the end goal – her successful transplant and healthy recovery. I looked at the journey in three parts:
- Pre-transplant
- Transplant/hospital stay
- Post-transplant
My goal was to have as much of her daily care and needs become second nature to me prior to her hospital release. When she was released, the additional environmental interaction was familiar without the distraction of ‘everything new all at one time’.
What tools did you find useful as the caregiver and advocate?
I created a 3-ring notebook with tabs to manage spreadsheets, medical records/test, and doctor questions, so I could access information easily and quickly. I created a spreadsheet to track her medication schedule. The purpose was to help me identify what was needed, including dosage when refilling medications both inside and outside the hospital. Click here to view medication tracker template. (For an Excel spreadsheet version of the attached please email kmichael@mpnadvocacy.com).
I also knew there was a good possibility that after her hospital release and within the first 100 days, she would have a trip to the emergency room and be re-admitted to the hospital. Therefore, medications and ‘the notebook’ were kept in one location and easily picked up and transported with us. The notebook was with us each time we visited the care team.
I created additional spreadsheets to help track:
- Food and water daily intake and output. This is useful for doctor & nutrition appointments.
- Daily stats: blood pressure, temperature, pain levels, exercise, spirometer therapy. This is useful for tracking blood pressure and temperature anomalies. Because if her temperature rose to a specific number, she had to go to the emergency room immediately.
- Signs of graft vs host disease (GVHD).
- I choose to stay in the hospital 24/7 to understand how the nursing staff/care team handled her care. This experience helped me understand her routine.
- I figured if I learned her hospital routine, it would be familiar when she was released.
- I used my smartphone and set alarms with labels so I knew what drugs were due when. (Used upon hospital release.)
- I utilized Caring Bridge (www.caringbridge.org) to communicate Andrea’s transplant journey to her friends and family. My intent with each post was to create an engaging story yet convey “a day in her life” so everyone could get a sense of being there.
What was the most challenging part of your role and why?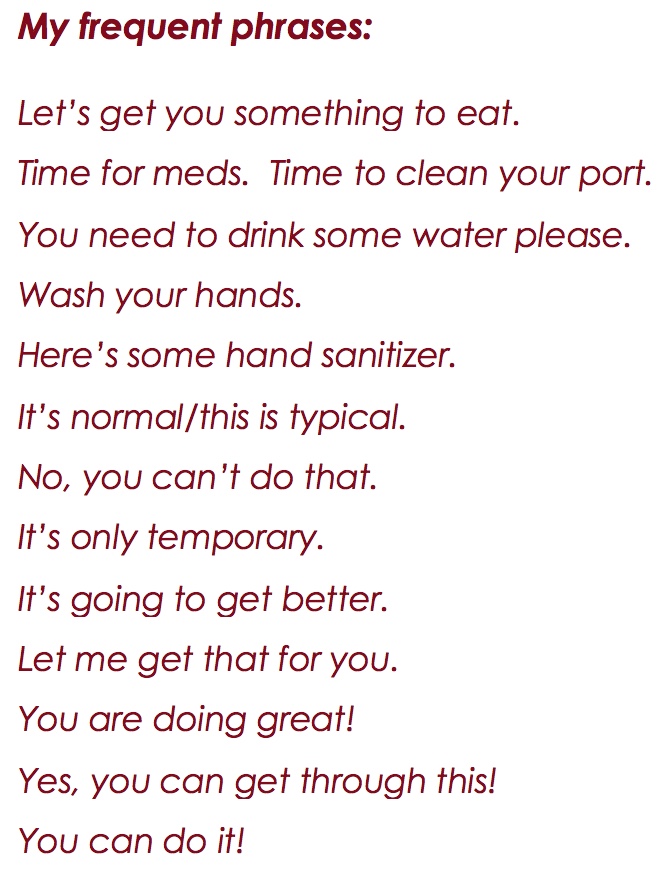
Coming home and changing environments automatically kicked us back to normal behaviors and patterns. I felt we had to be more careful and diligent in preventing infection. Even though we were home, I had to be more watchful because familiarity brings about a relaxed state. Her immune system was developing and the risk of infection was too great. Andrea quickly tired of me saying “No, you can’t do that or touch that.”
Once home, Andrea’s friends visited. This was a considerable risk to her because the natural tendency is to hug and touch. To reduce her risk, we asked people to use hand sanitizer when they were around her. We developed a routine where I would greet her friends first with a hug and explain she couldn’t hug yet. Andrea stood back a few feet to reduce her availability.
What I learned :
Every recovery and journey is different.
While it’s tempting, don’t measure your progress against someone else. It’s your journey. That goes for both the patient and caregiver!
The “notebook” was a great tool. It kept us on schedule for all medications and were able to provide information to the doctors as needed.
The hospital care team staff is a critical part of your recovery. Don’t opt for staying close to home if you feel a facility’s care team is better in another location.
Deciding where to have the transplant included researching the number of myleofibrosis transplants, versus other blood disease transplants, and the success that facility had.
Participate in the journey. I chose to shave my head at the same time Andrea did. It sure made showering quick and easy!
Take in the outdoors and/or change the scenery.
Exercise or go for walks. Listen to music. Visit a friend. Go to the grocery store. Do something to clear your head and regain perspective.
Have a confidante. It’s normal to question, or become frustrated, and to second guess. But remember – it’s temporary.
You are the coach, cheerleader, and guardian all at once. Embrace the many hats you will wear!
Click here to read Andrea’s Transplant Story
MPN Patient Daily Stats 06-10-18
