DISCUSSION QUESTIONS
- How do you monitor and manage anemia in patients with primary myelofibrosis prior to starting Janus kinase (JAK) inhibitor therapy?
- While receiving a JAK inhibitor therapy?
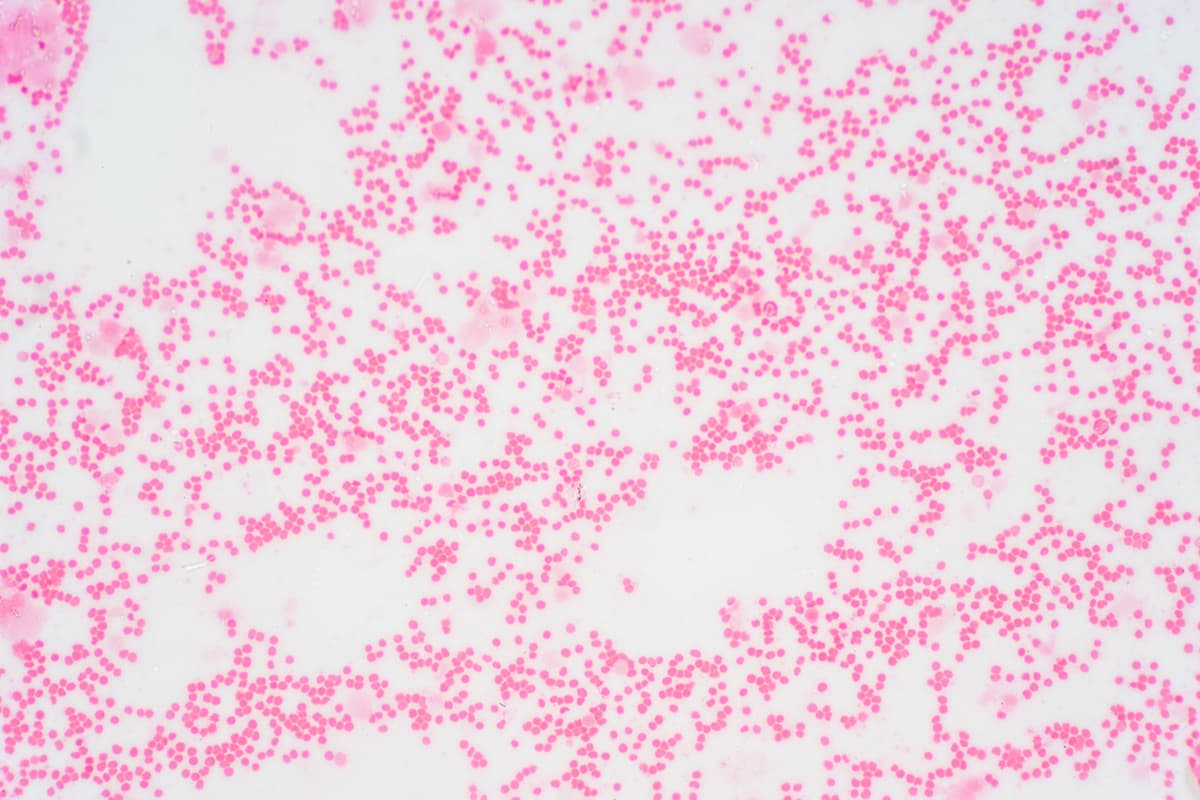
Andrew Kuykendall, MD: How do you monitor and manage anemia in patients with myelofibrosis even prior to starting a JAK inhibitor? If you’re initially evaluating someone, they come in with hemoglobin of 7 or 8 g/dL or something like that, how does that impact your thinking, and how do you work that up?
Lazaros Lekakis, MD: The first thing is to make sure that they don’t have something easily fixable [such as] iron, B12, or folate deficiency. Theoretically, if you don’t have any nutritional cause or any immune causes, you could use erythropoietin analogs, but they are very tricky because they don’t help with the spleen, at least in my experience, and they may increase the risk of clots. I try to avoid them if possible. If I have to start a JAK inhibitor, if they have symptoms, either I go away from ruxolitinib [Jakafi] or I start a low dose of ruxolitinib. Sometimes I use anabolic steroids and prednisone. We have the thalidomide/prednisone [regimen] that now is kind of forgotten about.
Kuykendall: Erythropoietin-stimulating agents [ESAs] are limited in what they do, and certainly not helping other aspects of the disease. You did mention one of my favorite regimens, thalidomide/prednisone, which is looked over a bit nowadays, but has quite a potential for efficacy in terms of improving hemoglobin. But it’s probably something that’s gone by the wayside in many practices.
Luis Sumoza, MD: As Dr Lekakis says, there are some other options that you can use. Danazol is sometimes something you can use perfectly in this patient population. From the JAK inhibitors, there is momelotinib [Ojjaara]. But a priority for me is to refer a patient for a stem cell transplant; when I was a fellow, we did the first allogeneic bone marrow transplant at the University of Illinois, Chicago, and it was a very nice experience.
Kuykendall: [Dr Lekakis] also mentioned steroids, [and we are] thinking about things like danazol, androgen derivatives. We saw from the MOMENTUM study [NCT04173494] looking at momelotinib that danazol is an active agent.1 It was a large, randomized trial, one of the first randomized trials with danazol. The focus there was on momelotinib, but there’s also a lot to learn about what danazol could do as well from that study.
Sumoza: You’re mainly talking about anemia here, and [if], the patient is not a candidate for a transplant or a clinical trial [there are] the data about navitoclax/ruxolitinib, which basically double the response and reduction of the spleen.2
Kuykendall: Yes, these emerging therapies to some degree may change how we approach this disease. But I think that with some of these older therapies, especially when you’re when you’re first talking about someone who’s coming in with anemia, you need to think about ESA, danazol, and thalidomide/prednisone.
I think that ESA is probably the most prominently used. How many of you are checking serum erythropoietin levels in these patients to assess their candidacy for ESAs, is that a common practice?
Mukesh Kumar, MD: Yes, I’m checking on all of my patients.
Read more