November 15, 2024
Lisa Kuhns, PhD, MD
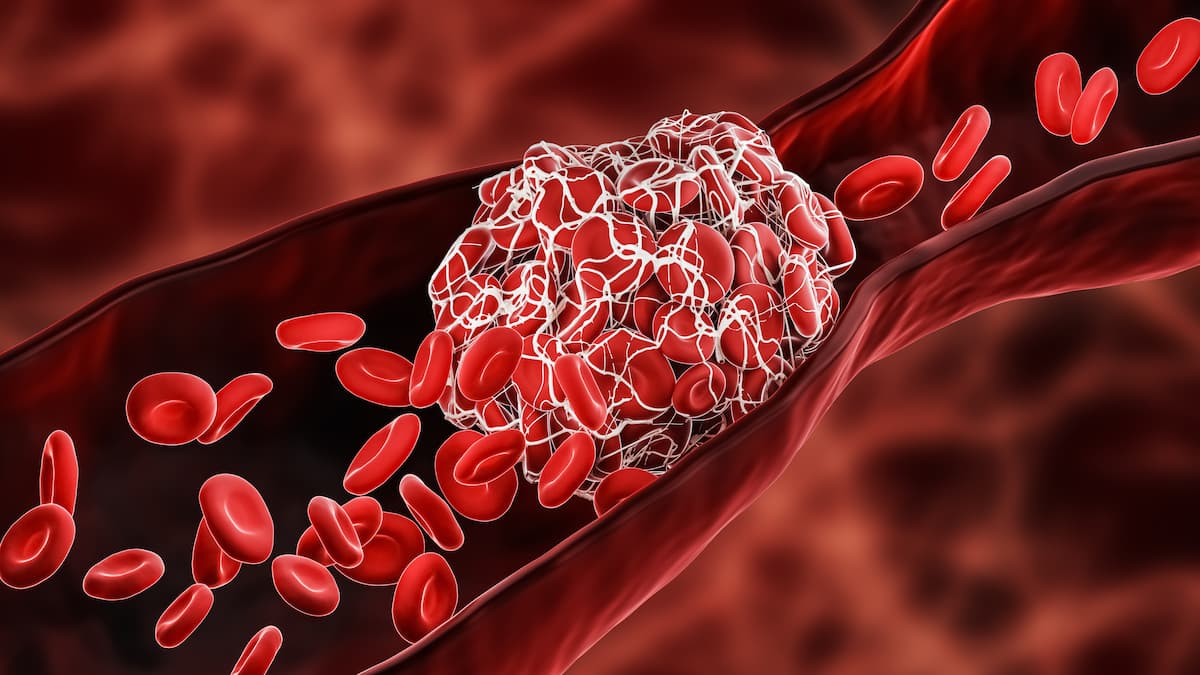
Despite the advancements in treatment, thrombosis remains a significant challenge for patients with myeloproliferative neoplasms (MPNs), contributing to increased mortality and the development of secondary cancers, according to an article published in Blood Cancer Journal.
“These risks arise from disease-related clonal hematopoiesis and subsequent chronic systemic inflammation, leading to thrombosis and genetic instability,” explained Tiziano Barbui, FROM, Fondazione per la Ricerca Ospedale di Bergamo ETS, Bergamo, Italy, and coauthors. “In our large databases of patients with MPN, we investigated the incidence and risk factors of thrombosis that may explain this association, culminating in an increased risk of mortality.”
Recent research has highlighted the persistent risk of thrombotic events in patients with classic MPNs, including polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF). These disorders are characterized by a high incidence of both arterial and venous thrombosis, which complicates patient management and contributes to disease progression. Notably, studies indicate that approximately 20% of MPN diagnoses are heralded by thrombotic events, with ongoing risks observed over time.
A large-scale study involving more than 9000 patients with MPN revealed significantly elevated hazard ratios for thrombotic events compared with matched controls. Specifically, arterial thrombosis hazard ratios were 3.0 at 3 months and 2.0 at 1 year postdiagnosis. Venous thrombosis rates were even more alarming, with hazard ratios of 9.7 at 3 months and 4.7 at 1 year. While conventional treatments such as hydroxyurea have demonstrated efficacy in reducing arterial thrombosis, their impact on venous events is less pronounced.
The implications of these findings extend beyond immediate health risks and suggest a potential link between thrombosis and progression to more severe forms of MPNs, such as myelofibrosis and acute leukemia. In particular, arterial thrombosis has been identified as an independent predictor of increased mortality in patients with ET and PV. For instance, a multistate model analysis indicated that patients experiencing arterial thrombosis had a 25% increase in mortality risk compared with those without such events.
Emerging evidence also suggests that thrombosis may be associated with an increased risk of developing secondary cancers in patients with MPN. A nested case-control study found that the occurrence of arterial thrombosis was independently linked to a higher incidence of secondary cancers, particularly among younger patients with MPNs. This correlation underscores the complex interplay between chronic inflammation induced by MPNs and the risk factors for both cardiovascular disease and cancer.
“We believe that arterial, and possibly venous thrombosis occurring during follow-up should be considered in the context of long-term occurring outcomes, including an increased incidence of solid tumors,” concluded the study authors.
Continued research is essential to unravel the underlying mechanisms linking thrombosis with disease progression and secondary malignancies, ultimately improving patient outcomes in this vulnerable population.
Reference
Barbui T, Ghirardi A, Carobbio A, et al. Thrombosis in myeloproliferative neoplasms: a viewpoint on its impact on myelofibrosis, mortality, and solid tumors. Blood Cancer J. 2024;14(1):188. doi:10.1038/s41408-024-01169-6
Read more