February 11, 2025
Author(s):
New study results published in the Journal of Translational Medicine reveal that circulating lactate is a key regulator of immune escape and bone marrow (BM) fibrotic transformation in patients with myelofibrosis (MF), with a marked increase in lactate concentration and lactate import channel monocarboxylate transporter 1 (MCT1) expression in the site of blood cell production. The investigators suggest that MCT1 blocking could be used as a novel antifibrotic strategy in patients with MF.1
Myelofibrosis can cause fibrosis in bone marrow. | Image Credit: © Jasmine – stock.adobe.com
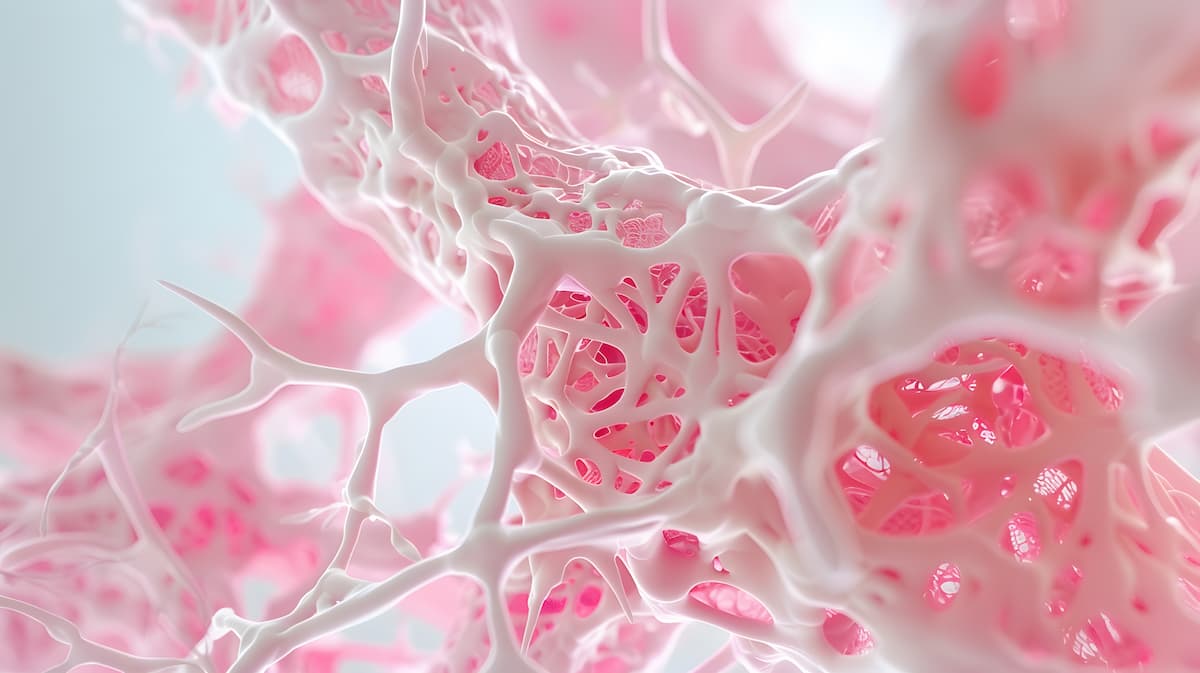
According to the study authors, the pathophysiology of MF is significantly influenced by alterations in the BM microenvironment, and these changes are often associated with the metabolic reprogramming of cancer cells in patients. Glycolysis is a hallmark aspect of the changes that occur in cancer cells; prior evidence from investigational models strongly suggests that lactate production is associated with tumor microenvironment (TME) progression in patients with certain types of cancer.1-3
Prior observations also indicate that increases in lactate dehydrogenase A (LDHA) have a central role in glycolysis, with high LDHA levels typically found in the sera of patients with MF, predicting shorter overall and leukemia-free survival. Within this context, excess lactate that is secreted by cancer cells can promote immune suppression and angiogenesis while also possibly playing a role in increasing the number of cancer-affiliated phenotypes (CAF), which promote fibrotic tumor formation, the investigators wrote.1,4
These authors sought to fill a gap in knowledge within the characterization of TME metabolic composition in patients with MF. Through their analysis, they demonstrated that the amount of circulating lactate increases in patients with MF, which eventually leads to the expansion of immunosuppressive subsets and the development of fibrosis. Furthermore, they observed that the expression of lactate export channel monocarboxylate transporter 4 (MCT4) in the TME becomes deeply remodeled during fibrotic transformation, “suggesting a link between lactate trafficking and pro-fibrotic establishment.”1