March 16, 2025
Author(s): Spencer Feldman
Fact checked by: Alex Biese
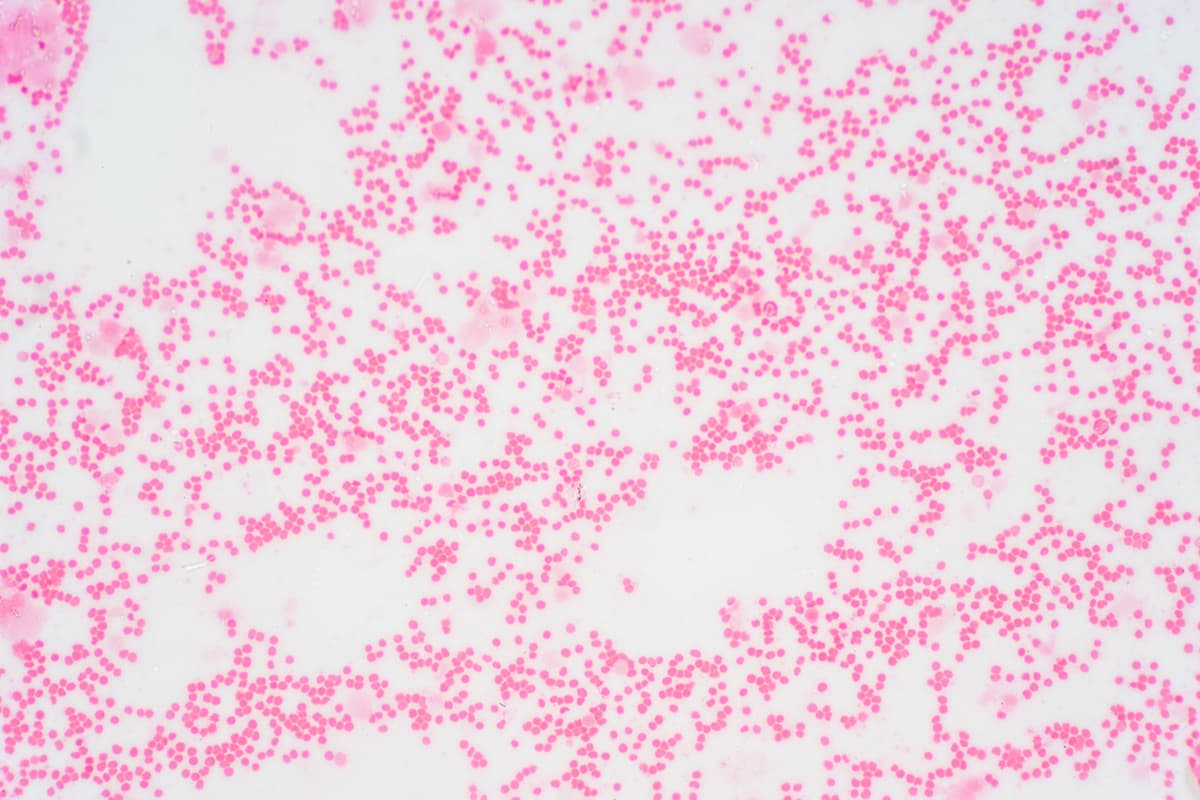
Among patients with calreticulin (CALR)-mutated myelofibrosis, real-world data reveal insights into those with splenomegaly and/or symptoms requiring therapy with Janus kinase 2 (JAK2) inhibitors.
The findings suggest that while Jakafi (ruxolitinib) shows some initial benefits, CALR-mutated patients may require more targeted and innovative therapeutic approaches for better long-term outcomes, according to study findings published in Annals of Hematology.
“Overall, despite the initial benefits of [Jakafi], CALR-mutated patients may require more innovative therapeutic interventions to achieve optimal outcomes. This further emphasizes the necessity of exploring alternative or adjunctive therapies tailored specifically for CALR-mutated individuals,” lead study author Dr. Francesca Palandri and colleagues wrote in the study.
Palandri is currently an adjunct professor primarily based in the Department of Experimental, Diagnostic and Specialty Medicine at the Università di Bologna, Bologna, Italy. She is also a junior researcher at Azienda Ospedaliero-Universitaria di Bologna, Institute of Hematology, Bologna, Italy.
Patients with CALR mutations began Jakafi with more severe disease, including higher peripheral blast counts, lower hemoglobin levels and worse marrow fibrosis, and after a longer median time from diagnosis (2.6 versus 0.7 years) compared to patients with JAK2 mutations. At six months, spleen responses were numerically lower in CALR-mutated patients, who also had lower rates of symptom responses (56.1% versus 66.7%, respectively). However, CALR-mutated patients experienced lower rates of high white blood cell counts.
Furthermore, in patients with delayed Jakafi initiation, anemia and reduced starting doses correlated with poorer survival. Managing anemia through interventions like danazol, erythropoiesis-stimulating agents, iron chelation and optimized Jakafi dosing may improve outcomes, according to study authors. The study also highlights the potential benefits of alternative JAK2 inhibitors with lower hematological toxicity.