November 21, 2022
Acquisition expands Merck’s growing hematology portfolio
RAHWAY, N.J. & SOUTH SAN FRANCISCO, Calif.–(BUSINESS WIRE)–Nov. 21, 2022– Merck (NYSE: MRK), known as MSD outside the United States and Canada, and Imago BioSciences, Inc. (“Imago”) (Nasdaq: IMGO) today announced that the companies have entered into a definitive agreement under which Merck, through a subsidiary, will acquire Imago for $36.00 per share in cash for an approximate total equity value of $1.35 billion.
This press release features multimedia. View the full release here: https://www.businesswire.com/news/home/20221121005295/en/
“We continue to invest in our pipeline with a focus on applying our unique capabilities to unlock the value of breakthrough science for the patients we serve,” said Robert M. Davis, president and chief executive officer, Merck. “This acquisition of Imago augments our pipeline and strengthens our presence in the growing field of hematology.”
Imago is a clinical stage biopharmaceutical company developing new medicines for the treatment of myeloproliferative neoplasms (MPNs) and other bone marrow diseases. Imago’s lead candidate bomedemstat (IMG-7289), an investigational orally available lysine-specific demethylase 1 (LSD1) inhibitor, is currently being evaluated in multiple Phase 2 clinical trials for the treatment of essential thrombocythemia (ET), myelofibrosis (MF), and polycythemia vera (PV), in addition to other indications.
“This milestone is a testament to more than a decade of pioneering research by Imago scientists and the entire Imago team’s unwavering dedication to improving the lives of patients,” said Dr. Hugh Y. Rienhoff, Jr., Founder and Chief Executive Officer, Imago BioSciences. “This agreement leverages Merck’s industry-leading clinical development expertise to maximize the therapeutic potential of bomedemstat while providing important value for shareholders. I would also like to acknowledge with gratitude the early investors – Blackstone Life Sciences, Frazier Healthcare, Omega Funds, Amgen Ventures, and MRL Ventures Fund who placed their faith in Imago beginning in 2014, as well as the outstanding study investigators and their patients who have made the clinical development of bomedemstat possible.”
“Evidence indicates that LSD1 plays an important role in the maturation of blood cells in the bone marrow,” said Dr. Dean Y. Li, president, Merck Research Laboratories. “We look forward to working with the Imago team to further investigate the potential of bomedemstat for patients with myeloproliferative neoplasms.”
Under the terms of the acquisition agreement, Merck, through a subsidiary, will initiate a tender offer to acquire all outstanding shares of Imago. The closing of the tender offer will be subject to certain conditions, including the tender of shares representing at least a majority of the total number of Imago’s outstanding shares, the expiration of the waiting period under the Hart-Scott-Rodino Antitrust Improvements Act and other customary conditions. Upon the successful completion of the tender offer, Merck’s acquisition subsidiary will be merged into Imago, and any remaining shares of common stock of Imago will be canceled and converted into the right to receive the same $36 per share price payable in the tender offer. The transaction is expected to close in the first quarter of 2023.
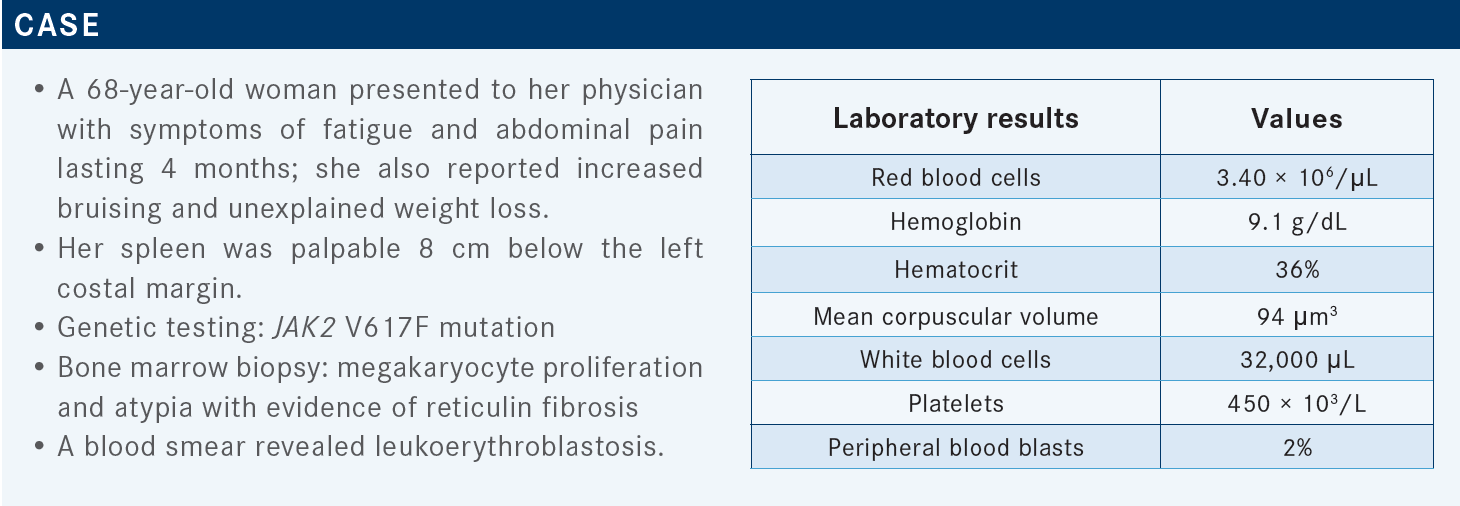
Myeloproliferative neoplasms
Myeloproliferative neoplasms are a group of diseases of the bone marrow characterized by excessive production of red blood cells, platelets, or certain white blood cells. Myeloproliferative neoplasms progress over time as the number of extra cells build up in the blood and/or bone marrow. This may lead to bleeding problems, anemia, infection, fatigue, thrombosis or other signs and symptoms. Certain myeloproliferative neoplasms may become acute myeloid leukemia (AML). Myeloproliferative neoplasms include chronic myelogenous leukemia (CML), polycythemia vera, primary myelofibrosis, essential thrombocythemia, chronic neutrophilic leukemia, and chronic eosinophilic leukemia.
About lysine-specific demethylase 1 (LSD1)
LSD1, also called KDM1A, discovered in 2004, is a member of a group of epigenetic proteins that regulate gene expression through chemical modifications of proteins, RNA and DNA. LSD1 regulates the maturation of bone marrow stem cells and is essential for the differentiation of progenitor cells into mature megakaryocytes and granulocytes and production of blood cells. Given the role that LSD1 plays in the function of malignant blood cells, targeting LSD1 for the treatment of blood cancers offers a new mechanism for the treatment of diseases associated with high morbidity and mortality.
Important Information About the Tender Offer
The tender offer described in this press release has not yet commenced. This press release is for informational purposes only and is neither an offer to purchase nor a solicitation of an offer to sell any shares of the common stock of Imago or any other securities, nor is it a substitute for the tender offer materials described herein. At the time the planned tender offer is commenced, a tender offer statement on Schedule (TO), including an offer to purchase, a letter of transmittal and related documents, will be filed by Merck Sharp & Dohme LLC (“Merck”) and M-Inspire Merger Sub, Inc., a wholly-owned subsidiary of Merck, with the Securities and Exchange Commission (the “SEC”), and a solicitation/recommendation statement on Schedule 14D-9 will be filed by Imago with the SEC. The offer to purchase shares of common stock of Imago will only be made pursuant to the offer to purchase, the letter of transmittal and related documents filed as a part of the Schedule TO.