By Ron K.
 Fortunately, my MPN journey has been a long one. I was first diagnosed 32 years ago and I know have post-Polycythemia Vera Myelofibrosis. Looking back it was almost archaic in nature. Today the progress has been immense on many fronts, not just in treatment, but with treating the patient as a whole. As many of you know, there is no exact recipe book for life with cancer and its treatment journey is unique. My hope is that sharing some of my experiences may help someone else along the way.
Fortunately, my MPN journey has been a long one. I was first diagnosed 32 years ago and I know have post-Polycythemia Vera Myelofibrosis. Looking back it was almost archaic in nature. Today the progress has been immense on many fronts, not just in treatment, but with treating the patient as a whole. As many of you know, there is no exact recipe book for life with cancer and its treatment journey is unique. My hope is that sharing some of my experiences may help someone else along the way.
There is a quote by Albert Einstein that reflects my approach to my medical journey
Learn from yesterday, Live for today, Hope for tomorrow. The important part is to not stop questioning.
Learn, Live, Hope – three good words for any cancer patient.
As those with an MPN know this is a chronic neoplasm and unfortunately there is no treatment yet to cure this illness. Some of the latest MPN and MF drugs do improve one’s quality of life and even appear to extend one’s survival, a significant milestone from what was available just a handful of years ago. Finding ways to slow or stop the progression is my only hope until medical knowledge can surpass me with a real solution.
Having a chronic cancer and having it for a long time has enabled and encouraged me to evolve into a healthier lifestyle. One does not have to change everything overnight but just evolve and continue to build healthier ways, one step at a time. While there is no evidence that a healthy lifestyle will cure me, it is something I can do and have control over.
This all started back in 1985 when I went to my family doctor with a cold and I mentioned that my colds seem to last longer and hit me harder than others. A simple blood test began my journey. I would not be alive today if I followed my first hematologist’s treatment plan. He wanted to treat me in a traditional manner at that time, with a radio isotope that kills off some of the marrow, they know now that treatment leads to an acute leukemia years down the road. Instead my intuition questioned this approach, since I was only 31 and I thought that I might need that marrow later in life. I called a major metro medical center and asked for an appointment with their Chief of Hematology. Unknown to me at the time, and not commonly termed in the 1980’s, I was going to get something called a second opinion. I got an appointment and his approach was quite different. He wanted to understand me, my rate of progression, severity, etc as that would lead him to figure out how to best treat me. He even commented that the current radio isotope treatment (my first hematologist’s plan) to kill off marrow was likely going away as he saw it.
Today, I am a patient of Dr. Mesa’s. I found that they could answer all my questions. Answers to questions that my previous hematologists could not answer. They have knowledge that is very leading edge as to direction of MPN treatments as they are part of an elite group of hematologists that are making many of the MPN discoveries, designing the clinical trials and studies with other key hematologists around the world. So my personal doctor advice is to make sure you find the right doctor and treatment strategy for you. Listen to your intuition and ask questions, seek information and acquire knowledge in your cancer and health. Expect answers or find those professionals that can give them to you. While I did not need a MPN specific doctor early on I do need one now as I am living well beyond the averages.
For me, finding the right doctor has been a key in my cancer treatment journey. Getting a second opinion is also key. What you will likely find is the different doctors will agree on the diagnosis but their treatment strategy will often be different.
I attend conferences, seminars, and special programs such as those that the MPN Advocacy and Education International puts on. I have done online webinars or conferences as well as belong to online MPN listing groups to learn and share information. I find this information to be helpful to ask the right questions to my doctors and understand what may be option in the future.
I believe support makes a difference. It is helpful to have support from your spouse, kids, parents or friends. I also find that support groups can be very helpful as well. As they can fill a support void that is missing from one’s non-cancer family and friends. This is no fault of family, spouses, or friends in that they do listen and they do try to understand and relate and they do support the cancer patient, but I have found that belonging to a cancer support group often helps to fulfill things non-cancer patients cannot quite grasp. I have belonged to both hematology specific support groups and all cancers support groups. You might want to try both and see if one works better than another.
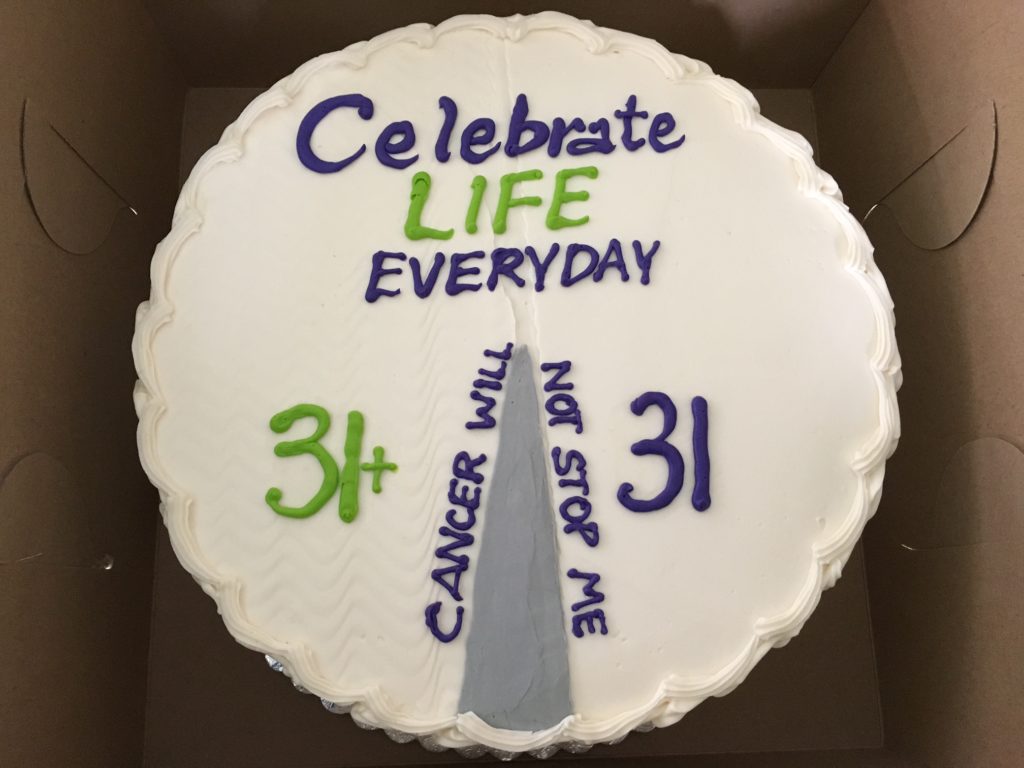
As I live my life, I am grateful for every day. Everyday is a great day, just some are even better than others. I even celebrated the point in my life where I have lived longer with cancer as part of my life than without cancer. That was at about 31 1/2 years and I had a bakery make me a cake to celebrate the occasion. The cake was symbolic of my MPN journey and view of life. I celebrated this occasion with my all cancer support group. So while cancer is a part of my life I run my life with cancer being a part of it and I do not let my cancer rule over me. I am hopeful that a cure is in our much sunnier MPN journey. May the best be yet to come, and enjoy the day!