Bill C. Veteran and MPN Patient
In January 2017, my husband, Bill, was enjoying his consulting business and writing a book that has been in his mind for years, when an annual physical changed everything. Some lab work was “off” according to the Veterans Administration (VA) physician so Bill sent the lab results to our personal physician, who is also our best friend. Within ten minutes after receiving it, our friend asked Bill to come to his clinic immediately. Further blood tests yielded an initial diagnosis of Chronic Myeloid Leukemia (CML).
While we were reeling from that shock and trying to ground ourselves, our physician friend sent us to a local hematologist for additional work-ups and treatment. Following a bone marrow test, we were further shocked to find out that the CML we had become somewhat resolved with was indeed Myelofibrosis (MF). We sat in a dumb stupor trying to figure out what that was, how serious it was, where it came from, what we could do about it, etc. We were encouraged to start on the only medication for Myelofibrosis, Jakafi, and were told the only drawback to the drug was its cost–$10,000/month! We immediately started working with the VA for them to supply the medication. After numerous telephone calls and in-person visits with both our hematologist and the VA (in a city 40 miles from our home), we secured VA support for Bill’s Jakafi. It now routinely comes to our home in an innocuous package. The initial symptoms Bill was experiencing responded to the Jakafi but so did the platelets and hemoglobin which are continuing to drop so we played with the dosage to, hopefully, continue to drive the white blood count down while keeping the platelet count and hemoglobin up closer to where they should be. The drop in Jakafi was too drastic and symptoms immediately returned so our local hematologist moved Bill back to the original dosage. Symptoms once again are gone and platelets somewhat controlled but still very low. Hemoglobin is recovering which is good.
 While all of this was going on, we decided, with the support of our local hematologist (who is wonderful realizing this is all about Bill and not about the hematologist’s ego), to go to Rochester, MN to Mayo Clinic to see one of the leading researchers in Myelofibrosis, Dr. Tefferi. While there was no proactive guidance offered from this visit, we did learn that we should only approach researchers whose field of study is a fit between their interests and Bill’s current health status. To that end, we went to Northwestern University in Chicago to see Dr. Brady Stein, another renowned Myelofibrosis researcher. He listened and answered all of our questions while assessing Bill’s fitness for ongoing clinical trials. His ultimate recommendation was for us to consider a transplant—again, another shock as we had hoped that we would have a variety of alternative treatments Dr. Stein is concerned that Bill’s Next Gen Sequence report that showed other mutations limit the time he will have before he converts to Acute Myeloid Leukemia (AML). Since Bill is in such good health right now (ironically), Dr. Stein found him to be amongst 10% of people with MF that even qualify for a transplant consultation and while a transplant is a “rough ride” encouraged us to explore it.
While all of this was going on, we decided, with the support of our local hematologist (who is wonderful realizing this is all about Bill and not about the hematologist’s ego), to go to Rochester, MN to Mayo Clinic to see one of the leading researchers in Myelofibrosis, Dr. Tefferi. While there was no proactive guidance offered from this visit, we did learn that we should only approach researchers whose field of study is a fit between their interests and Bill’s current health status. To that end, we went to Northwestern University in Chicago to see Dr. Brady Stein, another renowned Myelofibrosis researcher. He listened and answered all of our questions while assessing Bill’s fitness for ongoing clinical trials. His ultimate recommendation was for us to consider a transplant—again, another shock as we had hoped that we would have a variety of alternative treatments Dr. Stein is concerned that Bill’s Next Gen Sequence report that showed other mutations limit the time he will have before he converts to Acute Myeloid Leukemia (AML). Since Bill is in such good health right now (ironically), Dr. Stein found him to be amongst 10% of people with MF that even qualify for a transplant consultation and while a transplant is a “rough ride” encouraged us to explore it.
To that end, we have met with Dr. Tom Chauncey who is the Program Director at the VA in Puget Sound-who along with the University of Washington at Seattle are the number one transplant center (particularly for people with MF) in the country. Dr. Chauncey was very generous with his time and counsel and offered to work with us as we continue to explore transplant options. With Dr. Stein’s support, we also will meet with the Director of the Northwestern University Transplant Program, Dr. Mehta.
Simultaneously, we filed a VA benefits claim related to Myelofibrosis, believing Bill’s exposure to Agent Orange most likely caused this illness, but we were denied. Bill is a Vietnam Veteran having served in Quang Tri—I Corp from November, 1968 – November, 1969 and was exposed to Agent Orange/Dioxin. While compiling our appeal information, we found numerous Citations where the VA had granted benefits for veterans (on appeal) who have been diagnosed with Myelofibrosis due to exposure to Agent Orange, so will be using that information to move our claim forward. During the exploration for more information, we also discovered that the VA is finalizing a rule to add to the benefits structure Stem Cell Transplant coverage as well as treatment protocol to include myelosuppressive therapies of which Jakafi is one. This proposed change is set to take effect in FY18 (which begins as soon as October 1, 2017) which is exciting for veterans waiting for coverage of Myelofibrosis because, at least, some of the symptoms and associated therapies will be addressed.
MPN Advocacy & Education International continues to advocate for essential thrombocythemia, myelofibrosis and polycythemia vera to be included in the VA’s ‘presumptive’ list of illnesses related to Agent Orange exposure. Please click here if you are in the process of filing a claim or appealing a claim for more details.
Like many of you, we are sure, our world right now is exploring drugs in Phase II or III of clinical trials that are successful in producing remission in MF as well as other drug trials/existing drugs that will hold down the “blasts” that would otherwise convert Bill to AML. We are also exploring transplant centers, protocol, outcomes, experiences, etc. to get a better sense of whether that is something we even want to consider.
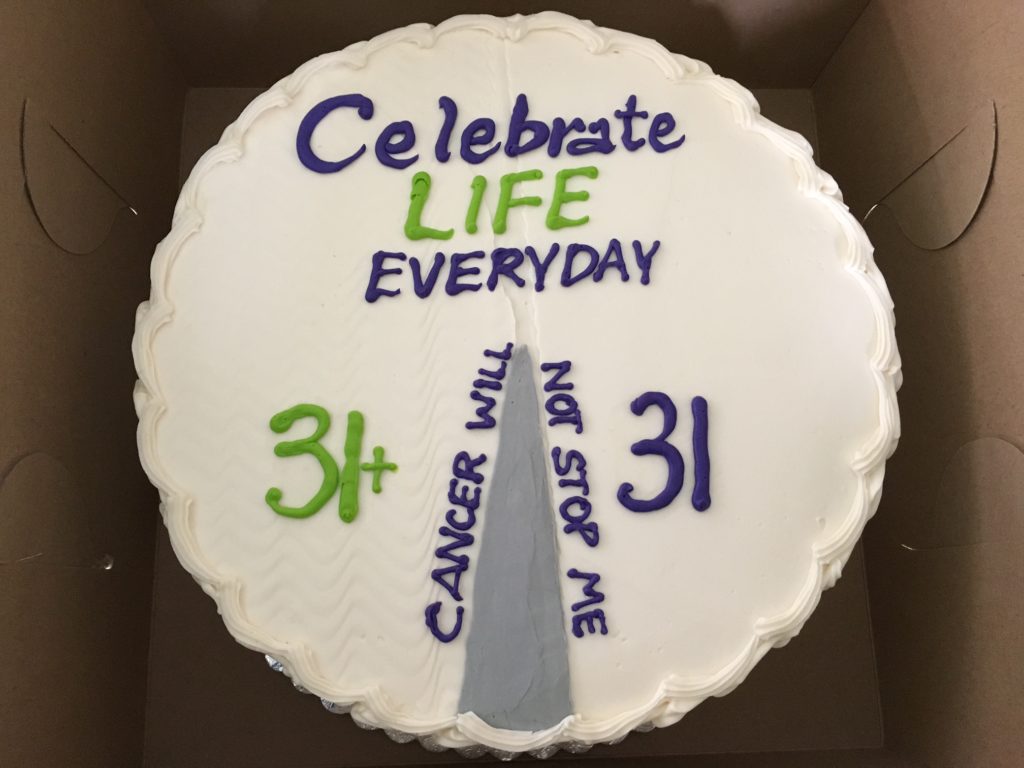
In the midst of all of this, we continue to work hard to enjoy our lives. Having a daughter with Down Syndrome who is now 43 years old taught us that nothing is ever guaranteed and that we would have to fight for anything and everything we wanted. We “cut our teeth” on the fights for our daughter, Mindie, against insurmountable odds and won. Now we are using those skills on Bill’s behalf. While sad and scared, we remain determined that there are many, many opportunities for Bill to remain as healthy as he is today and live a long and enjoyable life beyond the current prognosis. We know there is a lot to learn from all of you “in our same boat” and look forward to sharing stories and guidance between all of us. In the interim, all of you touched by an MPN are in our thoughts and prayers. Together we can change the face of these diseases!