January 27, 2025
Author(s): Luke Halpern, Assistant Editor
Cardiovascular risk factors (CVRFs) that increase thrombosis and overall mortality are more prevalent in patients with myeloproliferative neoplasms (MPNs), and especially those with myelofibrosis (MF), who have increased rates of hyperlipidemia and hypertension compared with patients with essential thrombocythemia (ET) or polycythemia vera (PV), according to study results published in Blood: Vessels, Thrombosis, and Hemostasis.1
Thrombosis is a potentially serious complication of myelofibrosis. | Image Credit: © Artur | stock.adobe.com
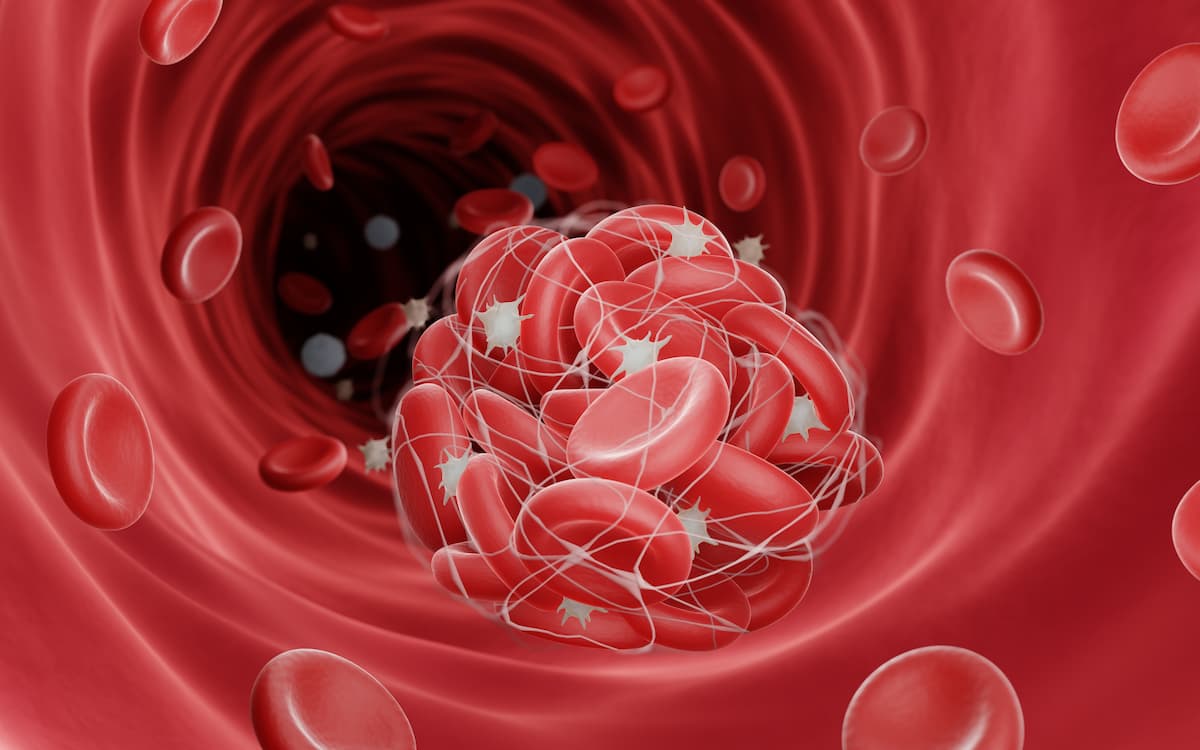
Managing thrombosis risk in patients with MF are pillars of optimal treatment, along with controlling bleeding. Studies have indicated that thrombosis is common across a variety of MPNs, including MF, ET, and PV, and more common in those patients when compared with the general population. CVRFs such as hypertension, hyperlipidemia, type 2 diabetes, and obesity have known effects on thrombosis in the general population, but data is unclear on the impact of CVRFs on patients with MF or other MPNs.2,3
For patients with MF, it is critical for pharmacists and treatment providers to recognize the prevalence of thrombosis and its potential risk factors, including CVRFs. In this current study, the investigators conducted a retrospective cohort analysis of 1005 patients with MPNs to evaluate the impact of CVRFs on real-world patient outcomes. Additionally, study authors investigated the likelihood of MPN transition to conditions such as MF or acute leukemia.1,2,3
Across the study sample, 215 patients had MF, 28 had pre-MF, 415 had ET, and 313 had PV. Patients with MF were found to be more likely to harbor at least 1 CVRF compared with those with ET, PV, and the general patient population (46% vs 34% in the general MPN population), according to the investigators. The most common CVRFs observed in the overall patient population were hypertension (21%), hyperlipidemia (16%), and having a body mass index (BMI) greater than or equal to 30 (12%). For patients with MF, these incidences were 31%, 22%, and 11% respectively.1
