Understanding Genetic Mutations in Myeloproliferative Neoplasms (MPNs)
A Quick Recap: What Are MPNs?
MPNs are a group of blood cancers that cause your bone marrow to produce too many blood cells. The three most common types are:
1. Polycythemia vera (PV) – where the body makes too many red blood cells.
2. Essential thrombocythemia (ET) – where the body produces too many platelets.
3. Primary myelofibrosis (PMF) – characterized by scarring of the bone marrow, which can lead to anemia, fatigue, and other complications.
A key driver of these conditions is genetic mutations, which affect how your blood cells grow and develop.
What Are Genetic Mutations?
A genetic mutation is a change in the DNA sequence. DNA is the instruction manual that tells our cells how to function, grow, and repair themselves. When a mutation occurs, it can disrupt these instructions and cause cells to behave abnormally—such as producing too many blood cells, which happens in MPNs.
Somatic Mutations and MPNs
Most of the genetic mutations associated with MPNs are somatic mutations. But what exactly does that mean?
● Somatic mutations are genetic changes that occur after birth, rather than being inherited from a parent. These mutations happen in specific cells, such as blood cells, and are not passed on to children.
● In the case of MPNs, somatic mutations occur in the hematopoietic stem cells—the cells in your bone marrow responsible for producing blood cells. When these stem cells acquire mutations, they can start producing too many blood cells, leading to the development of an MPN.
Understanding that MPNs are driven by somatic mutations is important because it helps explain why people develop these conditions later in life and why the mutations only affect blood cell production rather than all cells in the body.
Key Genetic Mutations in MPNs
There are several genetic mutations commonly associated with MPNs. The three most important ones to understand are JAK2, CALR, and MPL. Let’s take a closer look at each:
1. JAK2 Mutation (Janus Kinase 2)
○ What it is: JAK2 mutations are the most common genetic changes seen in MPNs, particularly in PV, where it’s found in about 95% of patients. It’s also present in approximately 50-60% of people with ET or PMF.
○ What it does: The JAK2 gene plays a key role in regulating blood cell production. When mutated, it sends constant signals to produce blood cells—even when your body doesn’t need them. This can lead to the overproduction of red blood cells, platelets, or other blood cells, depending on the type of MPN.
○ What it means for you: If you have a JAK2 mutation, your treatment plan may include JAK inhibitors, a type of medication that can reduce the activity of the mutated gene and help control your blood cell counts.
2. CALR Mutation (Calreticulin)
○ What it is: CALR mutations are found in about 20-25% of patients with ET and PMF, but not in PV. This mutation is the second most common genetic change in MPNs.
○ What it does: CALR mutations lead to overproduction of platelets or scarring of the bone marrow, depending on your specific condition. However, patients with CALR mutations tend to have a more favorable prognosis compared to those with JAK2 mutations, particularly in PMF.
○ What it means for you: Knowing that you have a CALR mutation can help guide your treatment options and give insight into your likely disease course. People with this mutation tend to have lower risks of blood clots compared to those with JAK2 mutations.
3. MPL Mutation (Myeloproliferative Leukemia Virus Oncogene)
○ What it is: MPL mutations are found in about 5-10% of patients with ET or PMF, but are not usually associated with PV.
○ What it does: MPL mutations cause abnormal signaling in blood cell production, similar to JAK2. This results in an overproduction of platelets and can contribute to bone marrow scarring in PMF.
○ What it means for you: MPL mutations are less common, but knowing you have this mutation can help your healthcare provider tailor your treatment and monitoring strategy, particularly when managing PMF.
Other Less Common Mutations
In addition to these key mutations, there are other genetic changes that can occur in MPNs, including ASXL1, TET2, and EZH2. These mutations are often referred to as “high-risk mutations” because they can affect the severity of the disease and the likelihood of progression to more serious conditions, such as acute myeloid leukemia (AML).
If you have one or more of these additional mutations, your doctor may recommend more aggressive monitoring or treatment to prevent complications.
Why Do Genetic Mutations Matter in MPNs?
Understanding your genetic mutation can give you important insights into your condition. Here’s why it matters:
● Prognosis: Some mutations are associated with a more aggressive disease course, while others may indicate a more stable condition. For example, patients with CALR mutations often have a better prognosis than those with JAK2 or MPL mutations.
● Treatment Options: Certain treatments may be more effective depending on your mutation. For instance, JAK inhibitors are often used to manage patients with a JAK2 mutation, while other therapies might be considered for patients with CALR or MPL
mutations.
● Risk of Complications: The type of mutation you have may affect your risk of developing complications like blood clots, bone marrow scarring, or progression to leukemia.
How Are Genetic Mutations Detected?
Your healthcare provider can determine if you have a specific genetic mutation through a bone marrow biopsy or a blood test. Genetic testing is an important part of diagnosing and managing MPNs, as it helps to confirm the type of MPN you have and guides treatment decisions.
Moving Forward: How to Manage Your MPN Based on Your Mutation If you’ve been diagnosed with an MPN and your genetic mutation has been identified, here are a few things to keep in mind:
1. Ask Questions: Don’t hesitate to ask your doctor about your specific mutation and what it means for your condition. Understanding your mutation can help you make informed decisions about your care.
2. Personalized Treatment: Treatments are becoming more targeted based on the specific mutations driving your disease. Work with your healthcare team to find the best approach for your mutation.
3. Regular Monitoring: MPNs can change over time, so regular check-ups and blood tests are essential. This allows your healthcare team to adjust your treatment as needed based on any new developments.
4. Support: Dealing with an MPN can feel overwhelming, but remember you’re not alone. Joining support groups or seeking counseling can help you cope with the emotional aspects of your diagnosis.
Genetic mutations, especially somatic mutations, are the driving force behind MPNs,influencing how the disease behaves and how it can be treated. By understanding the role of mutations like JAK2, CALR, and MPL, you can take an active role in managing your condition.
Genetic testing provides a clearer picture of your specific type of MPN, allowing your healthcare team to personalize your treatment and monitor your disease effectively.

 1. Why did you choose hematology as a specialty, specifically MPNs?
1. Why did you choose hematology as a specialty, specifically MPNs?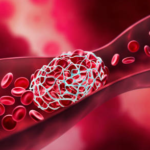 Thrombocytosis is significant in MPNs because one of the hallmark features of some MPNs, like Essential Thrombocythemia (ET), is the excessive production of platelets. This overproduction can lead to complications, such as blood clotting disorders, which can result in strokes, heart attacks, or other serious vascular issues.
Thrombocytosis is significant in MPNs because one of the hallmark features of some MPNs, like Essential Thrombocythemia (ET), is the excessive production of platelets. This overproduction can lead to complications, such as blood clotting disorders, which can result in strokes, heart attacks, or other serious vascular issues. By Natalie Giocondo
By Natalie Giocondo