Authors: Natasha Mathur, Andrew Chua Tiu, Ann Brazeau, Natalie Giocondo, Puneet Gill, Shanshan Liu, Guoqing Diao, Ramesh Subrahmanyam, Craig M Kessler, and Maneesh Rajiv Jain
Abstract
Background: Myeloproliferative Neoplasms (MPNs) profoundly affect patients’ well-being, necessitating effective symptom relief. Patient-reported outcomes are pivotal for care improvement, aligning with Centers for Medicare and Medicaid Services priorities. This study aims to assess MPN symptom burden among U.S. Veterans, examining risk levels, thrombo-hemorrhagic complications, medication use, information access, care, and service-connected benefits.
Methods: Conducted as a cross-sectional survey from December 1, 2023, – January 22, 2024, all Veterans in the MPN Advocacy Education & International database were recruited. Symptom burden was assessed using the validated MPN Symptom Assessment Form Total Symptom Score (MPN SAF TSS), with descriptive statistics and T-tests employed for analysis.
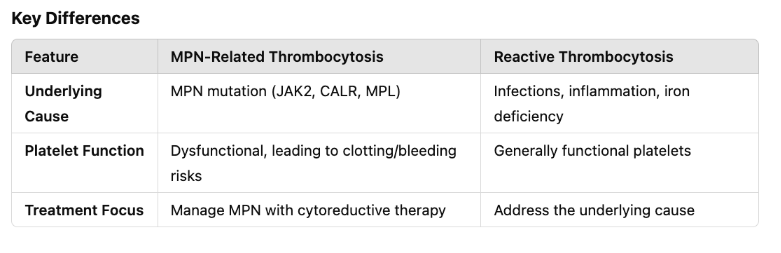
Results: Of 61 respondents, 88% were male, 92% Caucasian, 88% served during the Vietnam war. The mean age was 73±7, with MPN diagnosis at 64±9 and a mean duration of 44±10 years from service-connected exposure. Key findings included 56% Polycythemia Vera, 26% Essential Thrombocythemia, 16% Primary Myelofibrosis, 70% JAK2, 10% CALR, 3% MPL, 14% unaware of their mutation status, and 34% unaware of MPN risk status. Seventeen (28%) underwent phlebotomy, 64% used Hydroxyurea, 29% Ruxolitinib, and 3% Interferon. Fatigue and itching were the predominant and severe symptoms (Table), with 43% reporting no symptom improvement. Mean MPN SAF TSS of all respondents was higher than prior study by Emanuel et.al. which adjusted for MPN subtype (36.4 vs. 21.6, p<0.0001). Twelve (20%) reported bleeding and 10% reported venous thrombosis after MPN diagnosis, while 13% reported arterial thrombosis before MPN diagnosis. Twenty-two (36%) are not seeing an MPN specialist and 61% are not seeing a hematologist at their local Veterans Affairs Medical Centers. Twenty-three (38%) did not seek a second opinion while 43% do not have a caregiver. Respondents turn to MPN organizations (75%), physician offices (74%), Google Search (49%), Webinars (41%), and Facebook (23%) for information. Five (8%) received service-connected disability benefits.
Conclusions: Veterans with MPNs endure a substantial symptom burden, surpassing previous studies, signifying suboptimal management. Limited access to care persists, necessitating enhanced support. However, self-reporting bias and potential limitations in activity assessment must be acknowledged. Efforts to enhance MPN awareness, specialized care, and support mechanisms are imperative for comprehensive management.