For patients living with myeloproliferative neoplasms (MPNs), the term “thrombocytosis” often arises. While thrombocytosis—an elevated platelet count—is a hallmark of some MPNs like essential thrombocythemia (ET), it can also appear in other forms of MPNs or even due to unrelated secondary causes. Understanding the different contexts in which thrombocytosis occurs is key to effective management and improving quality of life.
Thrombocytosis in MPNs: A Common Feature
1. Essential Thrombocythemia (ET)
- Primary Cause of Thrombocytosis: In ET, the overproduction of platelets is driven by genetic mutations such as JAK2, CALR, or MPL in the stem cells of the bone marrow.
- Platelet Levels: Platelet counts in ET are persistently elevated, often exceeding 450,000/μL, and can reach over 1,000,000/μL.
- Risk of Complications: ET-associated thrombocytosis increases the risk of blood clots (thrombosis) and bleeding due to dysfunctional platelets.
2. Polycythemia Vera (PV)
- Secondary Thrombocytosis: PV primarily involves elevated red blood cell counts, but platelet counts are often high as well. This occurs because of the overactivity of the bone marrow, commonly linked to the JAK2 mutation.
- Complications: In PV, elevated platelets further amplify the risk of clotting, especially when combined with high red blood cell counts.
3. Myelofibrosis (MF)
- Variable Platelet Counts: In early stages of MF, thrombocytosis may occur due to hyperactive bone marrow. However, as the disease progresses and fibrosis (scarring) of the bone marrow develops, platelet counts often drop (thrombocytopenia).
- Implications: Elevated platelets in early MF contribute to the overall risk of thrombosis but are usually less prominent than in ET or PV.
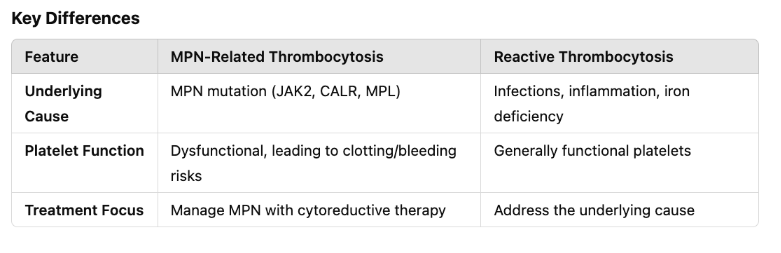
Thrombocytosis in MPNs vs. Reactive Thrombocytosis
MPN patients may also develop reactive thrombocytosis, where platelet levels rise due to an external trigger rather than the disease itself. This is important to differentiate, as the treatment approach varies.
Causes of Reactive Thrombocytosis in MPN Patients:
- Infection: Common colds, bacterial infections, or systemic inflammation.
- Iron Deficiency: Iron depletion, often seen in PV due to phlebotomy or blood loss, can elevate platelet counts.
- Surgery or Trauma: Any significant physical stress can temporarily increase platelet production.
- Inflammatory Conditions: Co-existing autoimmune diseases or inflammatory processes.
Managing Thrombocytosis in MPN Patients
For MPN patients, managing thrombocytosis involves addressing both the underlying condition and associated risks:
1. Medications to Control Platelet Levels
- Low-Dose Aspirin: Reduces the risk of clotting in patients with high platelet counts and cardiovascular risks.
- Cytoreductive Therapy: Drugs like hydroxyurea or anagrelide may be prescribed to reduce platelet counts in high-risk patients.
- JAK Inhibitors: For conditions like PV or MF with thrombocytosis, drugs like ruxolitinib target the underlying JAK2 pathway.
2. Monitoring and Prevention
- Regular Blood Tests: Monitoring platelet counts and clotting markers is crucial.
- Lifestyle Modifications: Staying active, avoiding smoking, and maintaining a healthy weight can help reduce clotting risks.
- Avoiding Triggers: Identifying and managing secondary causes like iron deficiency or inflammation can prevent exacerbation.
3. Managing Complications
- Clotting Risks: Thrombocytosis in MPNs increases the risk of strokes, heart attacks, and deep vein thrombosis (DVT). Prompt treatment of symptoms like chest pain, shortness of breath, or limb swelling is essential.
- Bleeding Risks: Paradoxically, MPN patients with thrombocytosis may experience bleeding due to abnormal platelet function, such as nosebleeds, gum bleeding, or gastrointestinal bleeding. Report unusual bleeding to your healthcare provider immediately.
Living with Thrombocytosis as an MPN Patient
Thrombocytosis in the context of MPNs requires long-term management, but there are steps you can take to improve your quality of life:
- Stay Informed: Learn about your specific MPN and its implications for thrombocytosis.
- Build a Support Network: MPNs are rare conditions. Connecting with support groups or online communities can provide emotional support and practical advice.
- Communicate with Your Care Team: Keep an open dialogue with your hematologist, and don’t hesitate to ask about treatment options, clinical trials, or lifestyle recommendations.
Thrombocytosis in MPN patients is more than just a high platelet count—it’s a complex condition with significant implications for your health. Understanding the nuances of your condition is essential for effective management, whether it’s caused by essential thrombocythemia, polycythemia vera, or reactive triggers. By working closely with your healthcare team and staying proactive in your care, you can navigate the challenges of thrombocytosis and live a fuller, healthier life.
